Updated: 11/3/23
Are you suffering from unexplained headaches, nasal congestion and other uncomfortable symptoms that don’t seem to have any obvious cause? You may be one of millions who suffer from histamine intolerance. This is an increasingly common condition — in fact, many people aren’t even aware they have it! But don’t worry: With the right supplements and treatments, you can find relief. In this blog post, we’ll look at how histamine intolerance works and explain some easy ways to reduce its effects on your health. Read on to learn more about how to manage this issue so that you can start feeling better fast!
What is Histamine?
Histamine is a chemical compound that exists in our bodies and is responsible for a wide range of functions. Although histamine is usually associated with allergies and inflammation, it plays an important role in our immune response and overall health. Understanding what histamine is and how it affects our bodies is an important step towards optimal health.
Histamine is a biogenic amine that is produced by our bodies and can be found in various foods. It is a neurotransmitter that plays an important role in our immune response, regulating gastric acid secretion, and controlling blood vessel permeability. Histamine is also involved in the regulation of sleep and wakefulness, as well as other physiological processes.
What is Histamine Intolerance?
Histamine intolerance is a condition that occurs when the body’s stores of enzymes responsible for breaking down histamine are not sufficient. This leads to a build-up of histamine in the body that can trigger allergy-like symptoms such as runny nose, watery eyes, itching, and hives. Additionally, high levels of histamine can expand the blood vessels, causing headaches, hypotension, and even vertigo.
Histamine intolerance can also affect digestive health, causing symptoms such as abdominal pain, bloating, diarrhea, and constipation. Other symptoms can include irregular heartbeats, flushing, and sleeping problems.
Histamine intolerance is often misdiagnosed due to the similarity of its symptoms to allergies and food intolerances. However, it is essential to differentiate between them because the management of each condition varies significantly. The best way to determine if histamine intolerance is the culprit behind your symptoms is to keep a food diary and eliminate high histamine foods to see if there is an improvement.
Histamine Intolerance Symptoms
Histamine intolerance is not a true allergy, but the symptoms it causes may be similar to an allergic reaction. Although they are not usually life-threatening, some of the symptoms can be severe. For example, it may cause:
Headaches or Migraines
If you frequently get headaches or migraines, it could be a sign of histamine intolerance. Histamine is a vasodilator, which means it can widen your blood vessels and cause headaches.
Digestive issues
Histamine can also cause digestive issues such as bloating, gas, diarrhea, and abdominal pain. If you notice that you feel worse after eating certain foods, especially those that are high in histamine, it could be a sign of intolerance.
Skin Reactions
Skin reactions are a common sign of histamine intolerance. You may experience itchiness, hives, eczema, or other skin rashes. These symptoms often occur after eating high-histamine foods, or when your body produces too much histamine in response to an allergen. To reduce your histamine levels, you can avoid foods like aged cheese, fermented foods, and alcoholic beverages.
Respiratory Problems
Histamine can also affect your respiratory system and cause symptoms such as sneezing, runny nose, and difficulty breathing. If you notice that you have these symptoms after eating certain foods, it’s worth investigating whether histamine intolerance is the cause.
Mood Changes
Finally, histamine intolerance can also affect your mood. You may experience anxiety, depression, irritability, or brain fog. If you notice that you have more mood swings after eating certain foods, histamine intolerance could be the culprit.
Hormonal Imbalances
Hormonal imbalances, particularly in women, can be a sign of histamine intolerance. Women may experience irregular periods, severe PMS, or even infertility. Studies have demonstrated that histamine and estrogen share a biochemistry pathway. High levels of histamine can result in estrogen dominance leading to hormonal imbalances.
Fatigue and Brain Fog
Histamine intolerance can cause fatigue, brain fog, and difficulty concentrating. This is because histamine affects your adrenal glands, which regulate stress hormones like cortisol. When your stress response is disrupted, it can lead to low energy levels and mental fatigue. To reduce your symptoms, try to avoid stressful situations, practice stress-management techniques, and get enough sleep.
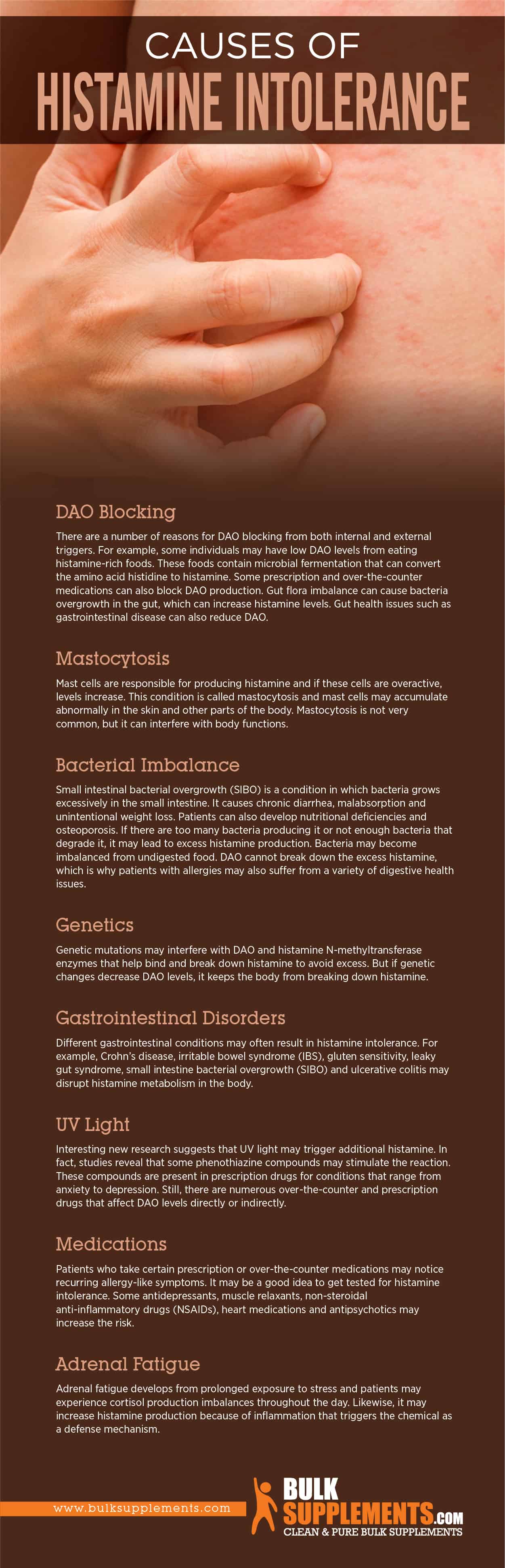
Causes of Histamine Intolerance
There are several factors that may result in histamine intolerance. It may result from DAO blockage and bacterial overgrowth. The body may also overproduce the chemical or have an inability to break it down properly.
Genetics
Your genes could play a significant role in histamine intolerance. If your family has a history of autoimmune diseases, migraines, eczema, or allergies, you could be at risk of developing intolerance. These conditions could be an indication of a genetic predisposition to intolerance. It’s worth noting that a person’s gut health can also have an impact on this condition.
Food Sensitivities
Certain foods contain high levels of histamine, and if you already have a high histamine level in your body, consuming these foods could trigger intolerance symptoms. Foods with high histamine levels include aged cheeses, alcohol, fermented vegetables, and canned fruits. If you have a sensitive digestive system, you might want to avoid some or all of these substances.
Allergies
Finally, the body’s immune response to allergies can create a histamine-rich environment, leading to symptoms that persist even after the allergen has been removed. So, if you experience seasonal allergies, for example, it’s worth considering that your intolerance could be exacerbated by the allergy season.
Medications
Some medications, such as analgesics, muscle relaxants, and anti-inflammatory drugs, contain histamine or block the production of an enzyme that breaks it down in the body. This action can cause an accumulation of histamine leading to an intolerance. If you’re using over-the-counter medications, always check the drug label for underlying ingredients that could trigger intolerance.
Gut Health
Your gut is home to billions of bacteria that help you digest food, absorb nutrients, and keep bad bacteria at bay. If there’s an imbalance in gut bacteria, you could develop intolerance. Poor gut health can result from a diet high in processed foods, alcohol and medication use or environmental factors. Incorporating a healthy, balanced diet and regular exercise can assist with good gut health.
Hormonal Changes
Women are more likely to develop intolerance. Changes in hormonal levels, such as those experienced during pregnancy, menstruation, and menopause, could trigger symptoms. This is because hormones like estrogen affect the body’s ability to break down it. If you’re a woman, it’s vital to pay close attention to your hormonal changes to identify potential intolerances.
Stress
Stress is a common trigger for intolerance, as it can stimulate its production and interfere with DAO activity. While you can’t always avoid stress, incorporating stress-reducing practices like meditation, mindfulness, or regular exercise can help alleviate the symptoms.
Gastrointestinal (GI) Disorders
Histamine intolerance is often linked to GI disorders such as leaky gut syndrome, irritable bowel syndrome, and inflammatory bowel disease. When the lining of your intestines is damaged, undigested particles and bacteria can leak into the bloodstream, which triggers the release of it. Over time, this chronic inflammation can lead to the development of intolerance.
Bacterial Overgrowth
Bacterial overgrowth in the intestines can also cause intolerance. Our gut is home to trillions of bacteria, and when there is an imbalance, certain strains of harmful bacteria can thrive and produce histamines. This can happen when we take antibiotics, which kill off good bacteria and allow bad bacteria to thrive. Other causes of bacterial overgrowth include stress, poor diet, and a weakened immune system.
Enzyme Deficiency
Histamine intolerance can also be caused by a deficiency in the enzymes responsible for breaking down histamine. When we eat foods that contain it, the DAO (diamine oxidase) enzyme works to break down it in the digestive tract. However, if there is a deficiency in DAO or other histamine-metabolizing enzymes, it can accumulate in the body and cause symptoms.
UV Light
Interesting new research suggests that UV light may trigger additional histamine. In fact, studies reveal that some phenothiazine compounds may stimulate the reaction. These compounds are present in prescription drugs for conditions that range from anxiety to depression. Still, there are numerous over-the-counter and prescription drugs that affect DAO levels directly or indirectly.
Adrenal Fatigue
Adrenal fatigue develops from prolonged exposure to stress and patients may experience cortisol production imbalances throughout the day. Likewise, it may increase the production because of inflammation that triggers the chemical as a defense mechanism.
Histamine Intolerance in Menopause
Menopause can be a tricky and tumultuous time for women, where the body goes through several different changes. One of the lesser-known side effects of menopause is histamine intolerance. It is a naturally occurring compound found in various foods, and our bodies also produce it in response to allergens. Intolerance can cause a range of symptoms, from mild to severe, such as headaches, skin rashes, diarrhea, and more.
The first question that comes to mind is, why does menopause cause intolerance? The exact reason for this is not entirely clear, but there are a few theories. For starters, estrogen regulates the release it in our bodies. During menopause, when levels of estrogen drop, it could lead to an increase in the production. Additionally, menopausal women are often more susceptible to gastrointestinal issues and gut imbalances, which can lead to a higher level of it in their system.
Histamine Intolerance and ADHD
When your body is unable to process excess histamine, it can overload your system and cause various reactions. One study suggests that high levels of it in the body can lead to an increase in ADHD symptoms, including hyperactivity and impulsivity.
Moreover, foods that are high in histamine can also trigger ADHD symptoms. Foods that are high in histamine include tomatoes, spinach, avocados, fermented foods, and alcoholic beverages. Dairy products, soy, and wheat can also trigger the release of it in the body. If you have ADHD, it is advisable to identify your trigger foods to manage your condition effectively.
What is a Low Histamine Diet?
A low histamine diet is designed to decrease the amount of histamine in one’s diet, reducing the symptoms of intolerance. The main goal is to avoid foods that are high in histamine and those that contain histamine-releasing agents. Some examples of high-histamine foods include fermented foods, aged cheese, citrus fruits, and certain vegetables like eggplant and spinach. Histamine-releasing foods include alcohol, chocolate, and shellfish. A low histamine diet targets these foods by providing alternative sources of nutrition, promoting cleaner, unprocessed diets, free of artificial preservatives and chemicals.
What Foods to Avoid on the Low Histamine Diet
When following this diet, it is important to avoid or limit the consumption of high histamine foods, as well as those that trigger the release of histamines in the body. Some examples of foods to avoid include:
- Fermented foods (e.g. kimchi, sauerkraut, pickles)
- Aged or cured meats
- Cheese
- Alcohol
- Vinegar
- Citrus fruits
- Tomatoes
- Soy sauce
In addition to these foods, it is also important to be aware of foods that are high in histamine-releasing compounds, such as strawberries, pineapple, and cocoa.
What Foods to Include on the Low Histamine Diet
While there are some foods to avoid on the diet, there are also plenty of foods that are safe to eat. Some examples of low histamine foods include:
- Fresh fruits and vegetables
- Fresh meats and fish
- Non-dairy milks (e.g. almond milk, coconut milk)
- Gluten-free grains (e.g. rice, quinoa)
- Herbs and spices (e.g. basil, turmeric, ginger)
Concerns and Precautions
Although the low histamine diet has shown notably positive results for digestive discomfort and other symptoms related to intolerance, it’s important to make some precautions. There’s a risk of some nutritional deficiencies if the diet is too restrictive or not followed correctly. Some people report feeling sluggish in the beginning stages, but proper planning and general education can help to avoid such initial struggles. Strict diets should also be avoided in pregnant or nursing women. Additionally, it may be necessary to consult with a nutritionist while following the low histamine diet, as nutritional changes should be prescribed accordingly to one’s individual needs.
Histamine Intolerance Diagnosis
While there is no definitive test for this intolerance, there are some biomarkers that can indicate a problem, such as elevated serum histamine levels, reduced levels of the enzyme DAO (diamine oxidase) responsible for breaking down histamine, and the presence of specific immune system markers such as IgE antibodies. However, these tests are not widely available and are often not covered by insurance. Therefore, the most reliable diagnostic tool is a food elimination trial combined with symptom tracking.
How Long Does Histamine Intolerance Last?
The duration of intolerance can vary depending on several factors, including the severity of the intolerance, the root cause of the intolerance, and the individual’s response to treatment. Mild cases of the intolerance may only last a few days to a few weeks, while severe cases can last for months or even years. It is important to understand that individual body responses vary from person to person.
Histamine Intolerance Treatment
Dietary Changes
A large part of managing and treating intolerance is avoiding factors that may trigger the symptoms. One of the most important management tools is making dietary changes and making conscious dietary choices.
Elimination Diet
This intervention is usually the first line of treatment for many patients. The elimination diet forces patients to avoid all foods high in it, foods that cause its release and those that block DAO for about one to three months. Next, physicians monitor the patient’s symptoms and assess how the body reacts.
Low Protein Diet
Histamines are made from amino acids derived from proteins. Bacteria and yeast turn the amino acid histidine into histamine, so protein can elevate levels in the body. This is a normal process, but if patients have a intolerance it can cause symptoms.
Medication & DAO Supplements
Aside from dietary changes, patients with the intolerance may also benefit from some medical treatments, depending on what causes the condition or the symptoms. In a small study, researchers used a small sample size of 14 participants and concluded that 13 of them experienced a decrease in symptoms after a daily dose of DAO supplement for about two weeks. Corticosteroids and antihistamine medications are common forms of treatment.
Patients can also try DAO supplements to manage the intolerance. However, the supplements will not cure the condition. But it can help metabolize what the patient consumes from food.
Probiotics
In many cases, patients with the intolerance may also suffer from damage to the digestive lining or excess bacteria that metabolize it. Therefore, the key step here is to rebalance the gut flora. Research states that probiotics may be an effective way to prevent and treat food allergies and food intolerances.
Histamine Intolerance Supplements
Ginger Root
As a rhizome, ginger root may be able to help deter allergic reactions. Apart from that, patients may also use it as an H2 inhibitor. It also has antioxidants and bioactive compounds that may help reduce inflammation in the body. Research states that ginger may also help support the digestive system, relieving nausea and vomiting. As a dietary supplement, the recommended dosage for ginger root extract powder is 1,000 mg once a day. Consult a doctor before taking this supplement. It may also cause heartburn, so take it with at least 8 oz. of water.
Mangosteen
Mangosteen may have effective healing powers thanks to its high antioxidant content. Since histamine intolerance can also develop from bacterial overgrowth, mangosteen’s antibacterial and anti-inflammatory properties may help combat different forms of yeast and bacteria in the body. Similarly, it may simultaneously reduce inflammation from allergies and bacterial overgrowth. In addition, various scientific studies note that mangosteen may be able to help reverse histamine-type allergic reactions in the body. The suggested serving size for mangosteen extract powder is 3,000 to 6,000 mg a day, or following a physician’s instructions.
Vitamin B6
Vitamin B6 plays an important role in the metabolism of it and can help to reduce histamine levels in the body. Studies have shown that high doses of vitamin B6 can alleviate symptoms of the intolerance, such as headaches and skin rashes. Consider taking a vitamin B6 supplement or increasing your intake of vitamin B6-rich foods, such as poultry, fish, and potatoes.
Vitamin C
Vitamin C can function as a natural antihistamine and boost the immune system. It is one of the most common immune-stimulating tools and patients often use it to prevent or treat the common cold and flu. It is a powerful antioxidant that can help protect the body from oxidative damage. According to studies, intravenous doses may also help treat allergic diseases and manage allergic reactions. As a dietary supplement, take 1,000 mg of vitamin C/ascorbic acid powder per day, if a doctor approves the dosage.
Butterbur
Butterbur is a plant extract that originates in Europe, Asia and some parts of North America and over the years, people used it to treat allergic rhinitis, or seasonal allergies. The National Center for Complementary and Integrative Healing (NCCIH) suggests that butterbur may have antihistamine properties. The recommended dosage for butterbur extract powder is 150 mg a day with water, after consulting a physician.
Nettle Leaf
Nettle leaf, a natural anti-histamine agent, has been widely researched for its histamine-blocking properties. It contains several bioactive compounds that prevent its release and efficiently quell intolerance. Nettle leaf tea can be a delicious and calming way to incorporate this supplement into your daily life. You can also purchase nettle leaf extract through us at Bulksupplements.com.
Quercetin
Quercetin is a natural antioxidant flavonoid compound in many foods and herbs, such as apples, broccoli, green tea, parsley, turmeric and red onions. According to research, quercetin supplementation may have anti-allergic and antihistamine effects. As a dietary supplement, the recommended serving size for quercetin dihydrate powder is between 250 and 500 mg once or twice a day. Consult a doctor before taking this supplement.
Omega-3 Fatty Acids
Omega-3 fatty acids are anti-inflammatory nutrients that can help to reduce inflammation and allergy symptoms. Studies have shown that omega-3 fatty acids can also reduce histamine levels in the body and alleviate symptoms of histamine intolerance. Consider taking an omega-3 supplement or increasing your intake of omega-3-rich fish, such as salmon, mackerel, and sardines.
Bottom Line
Histamine intolerance develops from a disequilibrium in histamine metabolism that causes the chemical to build up in the body. Histamine is a natural component in food that plays an important role in the central nervous system for communicating messages to the brain. It is also an important factor in immune defense. Symptoms of intolerance often mimic an allergic reaction, causing headaches, runny nose, itching and hives.
Histamine intolerance can be a sneaky condition as it can cause symptoms that are indirectly connected. Still, a bit of awareness and knowledge can help address the impacts on one’s daily life. There are ways to address intolerance symptoms, including dietary changes, avoiding high-histamine foods, and supplements or medication, so if you experience any of these symptoms, it’s worth talking to a medical professional. Remember, being in tune with your body can help you identify the early signs of histamine intolerance, allowing you to identify the root cause and take the necessary steps to preserve your well-being.
However, patients can also manage the condition by taking steps to avoid the triggers. It can cause a range of uncomfortable symptoms, but taking supplements that help to reduce histamine levels in the body can make a big difference. Consider adding vitamin C, quercetin, vitamin B6, probiotics, and omega-3 fatty acids to your supplement regimen to alleviate your intolerance symptoms. Always consult your doctor before starting any new supplement regimen to ensure your safety.
These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure or prevent any disease