Updated: 9/29/23
Are you living with the discomfort of arthritis and looking for relief? You’re not alone in trying to find ways to cope with this often painful chronic condition. The good news is that, while there’s no cure for arthritis, there are many proactive steps you can take to manage your symptoms. Our natural supplements have been carefully formulated to help reduce joint pain associated with rheumatoid arthritis and osteoarthritis by targeting inflammation at its source. With our supplements and a few lifestyle changes, you may find relief from your joints’ chronic aches and pains so you can get back to feeling like yourself again!
What is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is one type of arthritis and it is a persistent inflammatory joint condition. RA is an autoimmune disease, which means the immune system misinterprets the joint linings for “foreign” objects, so it attacks and destroys them. This leads to inflammation and pain.
Around 1.3 million people in the U.S. live with rheumatoid arthritis. In fact, a 2017 report shows that between 2004 and 2014, the condition increased significantly in the U.S., affecting around 1.36 million people in 2014. According to the Arthritis Foundation, women are 70 percent more likely to develop rheumatoid arthritis.
The most common symptom of rheumatoid arthritis is stiff joints, particularly after sitting down for a long time or upon waking up in the morning. Some individuals also often feel sick or fatigued and they may have a fever or loss of appetite.
Researchers have not discovered a specific cause for rheumatoid arthritis, but genes, hormones and environment can contribute. Treatment options include lifestyle changes, medication and surgery. These may stop or slow joint damage, as well as reduce swelling and pain.
Rheumatoid Arthritis vs. Osteoarthritis
Rheumatoid arthritis is different from osteoarthritis because it is an autoimmune disease, while osteoarthritis is progressive. RA develops from an overactive immune system that targets the joints and causes inflammation. The symptoms often appear quickly and worsen within a short amount of time. On the other hand, osteoarthritis is progressive, meaning it causes damage to the joints over time. It is caused by wear and tear on the joints and the symptoms usually only affect individual joints.
Can Rheumatoid Arthritis Go Away?
RA is a chronic condition that can be managed, but it cannot be cured. However, some people may experience periods of remission, which means their symptoms disappear or become much less severe. Remission can be temporary, and some people may experience flares of symptoms even after a long period of remission. On the other hand, other people may have a more severe form of RA that never goes into remission.
Symptoms of Rheumatoid Arthritis
RA symptoms can affect several different parts of the body and gradually wears away the bone. Although it may affect several different joints, they usually affect the hands (specifically the fingers and knuckles), wrists, shoulders, elbows, toes, knees, ankles and hips.
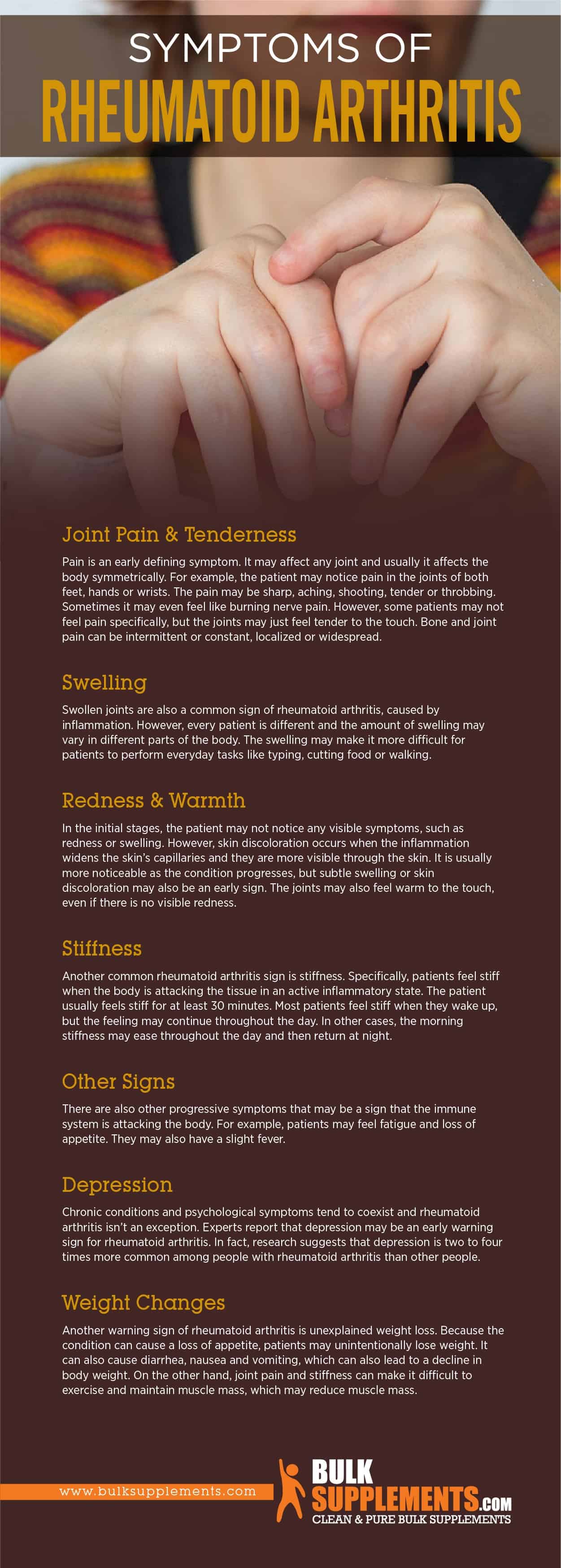
Joint Pain & Tenderness
Pain is an early defining symptom. It may affect any joint and usually it affects the body symmetrically. For example, the patient may notice pain in the joints of both feet, hands or wrists. The pain may be sharp, aching, shooting, tender or throbbing. Sometimes it may even feel like burning nerve pain. However, some patients may not feel pain specifically, but the joints may just feel tender to the touch. Bone and joint pain can be intermittent or constant, localized or widespread.
Swelling
Swollen joints are also a common sign of rheumatoid arthritis, caused by inflammation. However, every patient is different and the amount of swelling may vary in different parts of the body. The swelling may make it more difficult for patients to perform everyday tasks like typing, cutting food or walking.
Redness & Warmth
In the initial stages, the patient may not notice any visible symptoms, such as redness or swelling. However, skin discoloration occurs when the inflammation widens the skin’s capillaries and they are more visible through the skin. It is usually more noticeable as the condition progresses, but subtle swelling or skin discoloration may also be an early sign. The joints may also feel warm to the touch, even if there is no visible redness.
Stiffness
Another common rheumatoid arthritis sign is stiffness. Specifically, patients feel stiff when the body is attacking the tissue in an active inflammatory state. The patient usually feels stiff for at least 30 minutes. Most patients feel stiff when they wake up, but the feeling may continue throughout the day. In other cases, the morning stiffness may ease throughout the day and then return at night.
Other Signs
There are also other progressive symptoms that may be a sign that the immune system is attacking the body. For example, patients may feel fatigue and loss of appetite. They may also have a slight fever.
Depression
Chronic conditions and psychological symptoms tend to coexist and rheumatoid arthritis isn’t an exception. Experts report that depression may be an early warning sign for rheumatoid arthritis. In fact, research suggests that depression is two to four times more common among people with rheumatoid arthritis than other people.
Anemia
Anemia is a condition in which your body does not produce enough red blood cells, which can lead to fatigue and weakness. It is a common early symptom of RA, occurring in as many as 50% of cases. If you are experiencing unexplained fatigue or weakness, it may be anemia and worth discussing with your healthcare provider.
Eye Problems and Lung Complications
RA can occasionally affect other parts of the body, such as the eyes and lungs. Eye problems can include dryness, pain, redness, and sensitivity to light, while lung complications can include inflammation, fluid accumulation, and shortness of breath. These symptoms can be severe and require immediate medical attention.
Weight Changes
Another warning sign of rheumatoid arthritis is unexplained weight loss. Because the condition can cause a loss of appetite, patients may unintentionally lose weight. It can also cause diarrhea, nausea and vomiting, which can also lead to a decline in body weight. On the other hand, joint pain and stiffness can make it difficult to exercise, which may reduce muscle mass.
Why Rheumatoid Arthritis Causes Fatigue
RA is an inflammatory disease, meaning that the immune system mistakenly attacks healthy tissues, including the lining of the joints. This process releases chemicals called cytokines, which promote inflammation and pain. However, research has also shown that cytokines can affect the brain and central nervous system, leading to fatigue and other symptoms such as depression, anxiety, and cognitive impairment. In addition, inflammation can cause anemia, a condition in which the body produces fewer red blood cells than normal. This reduces the amount of oxygen that the blood can carry to the muscles and other organs, causing fatigue.
What Rheumatoid Arthritis Feels Like
Rheumatoid Arthritis can be an incredibly painful and difficult condition to live with. From constant pain and stiffness to fatigue, swelling, and emotional side-effects, the symptoms of RA can be overwhelming. However, with proper treatment and self-care, it is possible to manage the symptoms and maintain your quality of life. By understanding what rheumatoid arthritis feels like, you can be more informed and prepared to deal with the challenges of this condition. If you or a loved one have been diagnosed with RA, don’t hesitate to seek professional medical help and support. There are resources available to help you manage the condition and live a full and rewarding life despite it.
Complications from Rheumatoid Arthritis
Joint Damage
This is a serious complication from rheumatoid arthritis. According to a study from the University of Pennsylvania, individuals with rheumatoid arthritis had substantial deficits in muscle density and muscle mass compared to subjects without it. In chronic cases and without treatment, RA can damage cartilage and bone, causing joint deformity. If patients notice a significant decrease in strength, it’s important to contact a physician.
Rheumatoid arthritis can also increase the risk for heart disease and diabetes. Similarly, patients with RA who are also obese have an increased risk for heart disease. It can also affect patient’s employment because it limits mobility.
Cardiovascular Disease
One of the most significant complications of RA is cardiovascular disease. This is because the inflammation that causes joint damage can also damage the blood vessels that supply the heart. Over time, this can lead to an increased risk of heart attack, stroke, and other heart-related problems.
To minimize your risk of cardiovascular disease, it’s essential to manage your RA well. This includes taking your medications as prescribed, following a healthy diet, and getting enough exercise. Stop smoking, and limit alcohol intake.
Respiratory Issues
RA can also cause inflammation in the lungs, leading to problems such as shortness of breath and chronic cough. This is because the lining of the lungs can become inflamed due to the overactive immune system associated with the disease.
To manage respiratory issues caused by RA, it’s important to communicate with your doctor. You may need medications to manage inflammation in the lungs, and it’s essential to follow a healthy lifestyle that includes avoiding exposure to smoke and other irritants.
Depression and Anxiety
Finally, living with RA can take a toll on mental health. Many people with this condition experience depression and anxiety due to the pain and other complications associated with the disease.
To manage depression and anxiety caused by RA, it’s important to seek help from a mental health professional. You may also benefit from support groups and connecting with others who are living with this condition.
Risk Factors for Rheumatoid Arthritis
Medical research has not identified a specific cause for rheumatoid arthritis. However, there are different risk factors that may play a role, both genetic and environmental.
Genetic Risk Factors
Researchers have identified a connection between RA and the human leukocyte antigen (HLA). Specifically, HLA is a collection of genes that experts associate with the condition. It does not cause RA, but it increases the likelihood. However, not everyone with the HLA genes has RA. There is only a connection between them.
Gender
As mentioned earlier, RA affects women more than men. Besides, research suggests that women who have never given birth, or those who have given birth after the age of thirty-five, have a higher risk of developing the condition.
Obesity
While the link between obesity and rheumatoid arthritis is not completely clear, studies have suggested that there is a connection. People who are obese are at a higher risk of developing rheumatoid arthritis than those who are not. Additionally, those who are obese and already have rheumatoid arthritis may find that their symptoms are more severe or difficult to manage.
Infection
While it’s not entirely clear, rheumatoid arthritis may be triggered or exacerbated by infections. According to research, several viral and bacterial infections may increase your risk of developing RA. Early treatment of infections may help in preventing RA development or reduce its severity later on.
Environmental Risk Factors
Environmental factors do not cause RA, but if a patient already has a genetic predisposition—such as HLA genes—they can increase the risk, such as second-hand smoke, air pollution, silica mineral, bacteria or viruses and exposure to chemicals and mineral oils.
How Rheumatoid Arthritis is Diagnosed
Medical History
A proper diagnosis starts with a detailed medical history examination. Your doctor will ask you about your family history, and any relevant medical conditions you have had before. This is important because RA has a genetic component that makes it more likely for some people to get the condition.
Physical Exam
After taking your medical history, the next step is to examine the affected joints. The doctor will look for symptoms such as swelling, warmth, tenderness, redness, and joint deformation. Another important aspect of the physical examination is that your doctor will check for limited mobility in the joints. If they find any of these symptoms, then further tests will be taken to confirm or exclude RA.
Blood Tests
Blood tests are an important part of the diagnosis of RA. Laboratory tests are used to detect the inflammatory markers such as CRP (C-reactive protein) and ESR (erythrocyte sedimentation rate) in your blood. The presence of these markers indicates the presence of inflammation in your body, which is common in people with RA. Other tests that are commonly done include CBC (complete blood count), ANA (antinuclear antibodies), and RF (rheumatoid factor) tests.
Imaging
Imaging tests are also important in diagnosing rheumatoid arthritis. These tests help detect the presence of inflammation or joint damage. X-rays, MRI, and ultrasound are commonly used to detect joint changes.
Joint Aspiration
Joint aspiration is a less common test procedure used to diagnose RA. It is usually done on people who have not responded well to usual medication or whose symptoms suggest other inflammatory conditions. A needle is gently inserted into the joint, and synovial fluid is aspirated. This fluid is then sent to the laboratory to test for inflammation.
How Rheumatoid Arthritis is Treated
After a doctor makes a diagnosis, they can refer the patient to a specialist called a rheumatologist who will formulate a treatment plan. There is currently no cure for RA, but treatment aims to relieve pain and inflammation in the joints, prevent or slow down joint damage and minimize any dysfunction from pain, damage or deformity. Treatment options for rheumatoid arthritis may include medication, occupational therapy, surgery and lifestyle changes.
Medications
Some medications can help ease symptoms and slow down the disease’s progression. For example, non-steroidal anti-inflammatory drugs (NSAIDs) are available with or without a prescription in oral or topical forms. They help ease inflammation and pain. Corticosteroids are also powerful, fast-acting anti-inflammatory drugs that aim to slow progression. In addition, disease-modifying anti-rheumatic drugs (DMARDs) work to alter the course of rheumatoid arthritis.
Physical Therapy
Although medication may be effective, it cannot treat the pain and discomfort on its own. A doctor may also recommend physical therapy or exercise. With physical therapy, the patient can learn new, effective methods to perform daily tasks. This can ease stress on the joints. Low-risk exercises can also help reduce inflammation, even if exercise is painful.
Surgery and Joint Replacement for RA
In severe cases of RA, surgery may be required to repair or replace damaged joints. Surgery is usually recommended when non-surgical treatments are no longer effective. Joint replacement surgery involves removing the damaged joint and replacing it with an artificial joint made of metal, ceramic, or plastic. The most commonly replaced joints are the knee and hip, but other joints such as the shoulder, wrist, and ankle can also be replaced.
Lifestyle Changes
Rheumatoid arthritis affects many different components of everyday life, including work, social activities and leisure. Thankfully, there are many lifestyle changes to make that may help improve the quality of life in conjunction with other treatment methods.
Exercise
Exercise is one of the best ways to manage RA. It can improve your joint flexibility, strengthen your muscles, and reduce pain and stiffness. However, you need to be careful while choosing the exercise regime. Low-impact exercises such as swimming, cycling, walking, and yoga can be beneficial. It is also essential to warm-up before exercising and cool down after the workout to prevent injury. Physicians recommend 30 minutes of physical activity per day. Because RA increases the risk of other chronic diseases, such as heart disease and diabetes, exercise can help lower it.
Keep a Healthy Weight
There is no specific diet that can cure RA, but consuming a well-balanced diet can help manage symptoms. You can include foods that are rich in omega-3 fatty acids, such as fish, nuts, and seeds, which have an anti-inflammatory effect. It is also essential to avoid foods that can trigger inflammation, such as processed and fried foods, sugary drinks, and red meat. Consulting a dietician can be helpful in planning a healthy diet.
Obesity can cause complications for RA patients, potentially leading to high blood pressure and high cholesterol. It’s important to maintain a healthy body weight in order to stay healthy and better manage the symptoms.
Stop Smoking
Smoking is known to be a major risk factor for many diseases and conditions, and rheumatoid arthritis is no exception. People who smoke are at a higher risk of developing rheumatoid arthritis than those who do not. Additionally, for those who have a genetic predisposition for the condition, smoking increases the risk even further. Studies have found that smokers who have a particular genetic marker associated with rheumatoid arthritis are even more likely to develop the condition than nonsmokers with the same genetic marker. Smoking makes RA even worse and it can also increase the risk of other diseases. It may also interfere with exercise and weight loss.
Alternative Treatments for RA
Some people with RA turn to alternative treatments such as dietary supplements, acupuncture, and massage therapy to manage their symptoms. While some alternative treatments may be helpful, others have not been scientifically proven to be effective and may even be harmful. People with RA should talk to their healthcare provider before trying any new treatment or supplement.
Supplements for Joint Pain and Arthritis
Supplements might help RA patients by reducing pain and inflammation in the joints. Although they do not cure the disease or completely eliminate the symptoms, patients can use supplements in conjunction with other forms of medical treatment. Consult a doctor before starting a supplement regimen. They are not an adequate medical treatment. Instead, they simply aim to improve overall health.
D-Glucosamine Sulfate Potassium
The body produces glucosamine naturally from the amino acids glutamine and glucose. It’s required to produce glycosaminoglycan, a molecule that helps repair and develop cartilage as well as other body tissues. Research claims that consuming glucosamine sulfate may raise glucosamine levels in the blood in order to repair or reverse joint damage. One study showed that glucosamine was as successful as acetaminophen in alleviating joint pain. However, the study did not clarify whether the supplement increased joint function on its own.
Glucosamine and chondroitin are two of the most commonly used supplements for joint pain and arthritis.
It is also available as a dietary supplement. Take 1,000 mg of D-glucosamine sulfate potassium powder one to three times daily, or according to a doctor’s directions. Pregnant or breastfeeding women should discuss intake with a doctor.
Chondroitin Sulfate
Chondroitin sulfate helps support cartilage health. It also plays a role in preventing enzymes from damaging cartilage. Studies have shown that chondroitin can reduce joint pain and swelling, as well as increase mobility. It works by slowing down the breakdown of cartilage and promoting the growth of new cartilage. One study published in the Annals of the Rheumatic Diseases found that chondroitin supplements were more effective in reducing knee pain than a placebo.
Glucosamine and chondroitin are two supplements that are together to help reduce joint pain. Glucosamine is a compound that helps cartilage retain water while chondroitin helps provide cushioning in the joints. Together, they can help reduce inflammation and improve joint mobility.
A 2018 study even suggested that taking 800 mg of this supplement per day may be as effective in relieving joint pain as taking daily 200 mg doses of NSAIDs.
As a dietary supplement, take 750 to 1,500 mg of chondroitin sulfate powder per day, or based on a doctor’s directions.
Boswellia Serrata
Boswellia serrata has anti-inflammatory effects that experts believe may help ease joint pain. In fact, one study shows that boswellia can help relieve pain, swelling and increase mobility in patients with osteoarthritis or arthritis. Some participants experienced a drastic decrease in joint pain, which means boswellia may be as effective as prescription medications in treating arthritis or osteoarthritis.
The recommended dosage for pure boswellia serrata extract powder is 450 mg once or twice daily with food, after consulting a physician.
Devil’s Claw
Devil’s claw is a common treatment for skin diseases and it may contain anti-inflammatory properties. One study tested it on subjects with various rheumatic conditions and it appeared to significantly relieve pain in the subjects’ backs, knees, hips, shoulders, elbows, wrists and hands. In addition, most of the subjects in the study experienced an improved quality of life. In fact, 60 percent of the participants were able to reduce or stop using other pain medicines.
The recommended dosage for devil’s claw extract powder is 1,000 mg one to three times a day, unless a physician orders a different dosage.
Omega-3
Omega-3 is a type of fatty acid that is essential for good health. It is in fatty fish like salmon and mackerel, but it can be a supplement. Omega-3 has anti-inflammatory properties that can help reduce joint pain and stiffness. It can also help improve cardiovascular health. It is recommended to take an omega-3 supplement with a meal to prevent stomach upset.
SAM-e
SAM-e stands for S-adenosylmethionine, which is a compound that our bodies produce naturally. However, levels of SAM-e can decline as we age. SAM-e has anti-inflammatory properties and may help reduce joint pain and stiffness. It is a supplement for people with osteoarthritis, although more research is needed to fully understand its effectiveness.
Turmeric
Turmeric is a spice commonly used in Indian and Middle Eastern cuisine. It contains a compound called curcumin, which has potent anti-inflammatory properties. Studies have found that turmeric may help reduce joint pain and stiffness in people with osteoarthritis and rheumatoid arthritis. Turmeric supplements are available in capsule or powder form, and many people also add turmeric to their food as a spice.
Vitamin D
Vitamin D is known as the “sunshine vitamin” because our bodies can produce it when we are exposed to sunlight. However, many people do not get enough vitamin D from sunlight alone, particularly those who live in northern regions with limited sunlight. Vitamin D is important for bone health, and studies have shown that it may also help reduce joint pain and stiffness in people with arthritis.
MSM
MSM, or methylsulfonylmethane, is a compound that contains sulfur. It helps reduce inflammation and promote joint health by supporting the formation of collagen and other connective tissues. It helps to reduce pain and stiffness in people with osteoarthritis. You can take MSM as a supplement or get it naturally from foods such as onions, garlic, and cruciferous vegetables.
The Bottom Line
Rheumatoid arthritis (RA) is a chronic, disabling and progressive autoimmune condition. It causes pain, swelling and inflammation in and around joints and other organs in the body. Unlike osteoarthritis, the symptoms can appear very suddenly and they may affect any joint in the body. Usually the pain is symmetrical and patients experience pain in joints on both sides of their bodies.
There is no cure for rheumatoid arthritis, but treatments may help ease pain, reduce inflammation, slow down the disease’s progression and possibly prevent joint damage. Rheumatoid arthritis treatments include medications, occupational and physical therapy or surgery to prevent or repair damage to the joints. Physicians also recommend regular exercise to keep the joints strong and reduce inflammation.
Joint pain and arthritis can be debilitating, but with the help of supplements, you can reduce your symptoms and improve your quality of life. Omega-3s, glucosamine and chondroitin, vitamin D, turmeric, and MSM are just a few of the top supplements that can help alleviate joint pain and inflammation. As with any supplement, make sure to talk to your doctor before adding them to your routine, especially if you take other medications. With the right supplements, you can take control of your joint health and live a happier, more active life.
These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure or prevent any disease