Updated: 9/29/23
A peanut allergy can be serious and even life-threatening. It is important to understand the symptoms and how allergic reactions are treated. Even if you don’t have a confirmed allergy to peanuts, you might experience some signs or reactions when exposed. Whether this is your first time hearing about peanut allergies or it’s something you’ve been living with for years, learning more information can help keep you safe from allergic reactions. Let’s dive into understanding the signs of an allergic reaction, how these severe responses are treated, and ways that individuals with food allergies can still enjoy eating without putting their health at risk.
What is a Peanut Allergy?
A peanut allergy occurs when a person’s immune system has an abnormal, hypersensitive response to peanuts. Peanuts are one of the most common allergens and when ingested by people who are allergic, they can cause severe or life-threatening reactions.
Peanut allergies appear to be on the rise, especially in infants and young children. For example, between 2010 and 2017, reported cases of peanut reactions rose 21 percent in the United States. In some developed countries, up to 10 percent of young children may be allergic. Rates also seem to be rising in developing countries. Researchers are working hard to understand the reasons behind the increase in peanut allergies and develop new therapies to help those that have them.
While 20 percent of children outgrow their peanut allergy, most people have it for life. Understanding the signs of an allergic reaction and how to prevent exposure to peanuts remains the main focus of the overall management of peanut allergies in children and adults.
Can Peanut Allergy Go Away?
Peanut allergies typically develop during childhood and are known to persist throughout adulthood. However, research shows that approximately 20% of children with peanut allergies grow out of them. There is no guarantee that peanut allergy will spontaneously go away, but it is worth trying to reintroduce it to your diet to see if you are among the lucky few who grow out of it. Some researchers recommend introducing peanut products as early as 4-6 months of age to help reduce the risk of peanut allergies later on.
Symptoms of a Peanut Allergy
Symptoms of a peanut allergy can vary in severity. The way a person’s body reacts to peanuts on one occasion can be different from how it reacts on another occasion.
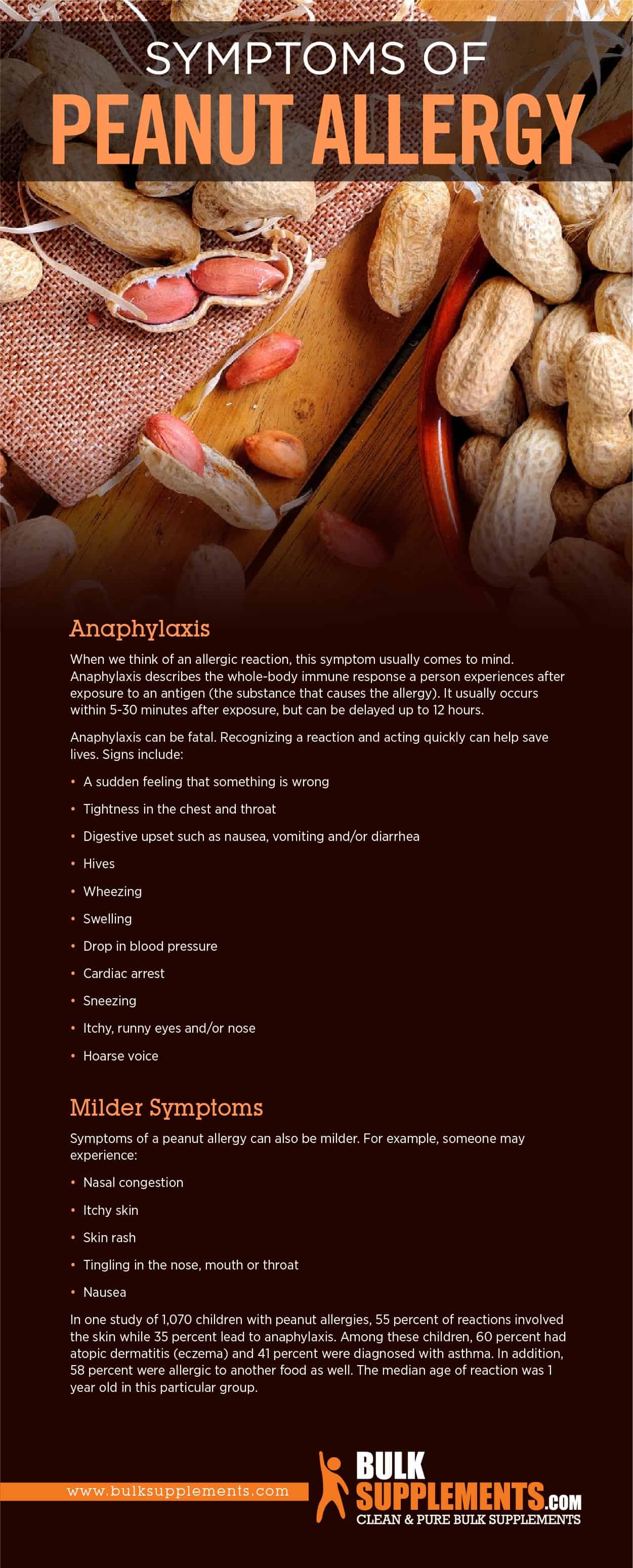
Anaphylaxis
When we think of an allergic reaction, this symptom usually comes to mind. Anaphylaxis describes the whole-body immune response a person experiences after exposure to an antigen (the substance that causes the allergy). It usually occurs within 5-30 minutes after exposure, but can be delayed up to 12 hours.
Anaphylaxis can be fatal. Recognizing a reaction and acting quickly can help save lives. Signs include:
- A sudden feeling that something is wrong
- Tightness in the chest and throat
- Digestive upset such as nausea, vomiting and/or diarrhea
- Hives
- Wheezing
- Swelling
- Sneezing
- Itchy, runny eyes and/or nose
- Hoarse voice
- Brain fog
- Fatigue
Milder Symptoms
Symptoms of a peanut allergy can also be milder. For example, someone may experience:
- Nasal congestion
- Itchy skin
- Skin rash
- Tingling in the nose, mouth or throat
- Nausea
In one study of 1,070 children with peanut allergies, 55 percent of reactions involved the skin while 35 percent lead to anaphylaxis. Among these children, 60 percent had atopic dermatitis (eczema) and 41 percent were diagnosed with asthma. In addition, 58 percent were allergic to another food as well. The median age of reaction was 1 year old in this particular group.
Cardiovascular Symptoms
While rare, some people may experience cardiovascular symptoms, such as a sudden drop in blood pressure and fainting. This is a sign of severe anaphylaxis that can lead to a sudden cardiac arrest, which is why it’s important to get immediate medical attention.
Can Peanut Allergy Cause Diarrhea?
While diarrhea is not one of the most common symptoms associated with peanut allergy, it can occur in some cases. When someone with peanut allergy consumes peanuts, the body’s immune response can lead to inflammation in the gut, resulting in diarrhea. The severity of the diarrhea can vary depending on the severity of the allergy and the amount of peanuts consumed. In some cases, diarrhea may be the only symptom of the peanut allergy.
Causes of Peanut Allergy
Peanut allergies occur when the immune system overreacts to the proteins in peanuts. The immune system then releases certain chemicals into the bloodstream, which causes the symptoms. Most reactions to peanuts result from eating peanuts or food made with peanut products.
Inhaling particles from peanuts (such as during the process of grinding, for example), can also cause a reaction. However, simply smelling the odor of peanuts or peanut butter is not believed to cause harm.
Similarly, coming into contact with a peanut usually doesn’t cause a reaction unless the person then touches his or her eyes, mouth or nose.
Risk Factors
Peanut allergies appear to be increasing worldwide. Researchers still don’t understand why, but they’ve identified some risk factors. Factors that put someone at a higher risk include:
- Age; children are more likely to develop a peanut allergy than adults
- Being male
- Having a family member with food allergies
- Vitamin D deficiency
- Living without pets and in an environment that is excessively sterile
- Antibiotic use
- Having eczema, asthma or seasonal allergies
- Being born in one country/culture and migrating to a new one, adopting the new culture’s diet and lifestyle
Allergies to Other Foods
Peanuts are not actually nuts, they are legumes. Other foods in the legume family include soybeans, peas and lentils. Tree nuts, on the other hand, include almonds, walnuts, brazil nuts, macadamia nuts, cashews, pistachios, pecans and chestnuts.
Having a peanut allergy does not increase your risk for having an allergy to other legumes, but does increase your risk of tree nut allergies by 25-40 percent. In addition, about 40 percent of children with food allergies in general are allergic to more than one food.
Allergy vs. Intolerance
While a food allergy stems from the immune system, a food intolerance is related to the digestive system. The two are often confused. A food intolerance can also cause very uncomfortable symptoms and require a dietary change but generally is not life-threatening.
Cross-Contamination
Cross-contamination occurs when peanuts come into contact with other foods or surfaces. This can happen during food preparation, packaging, or serving. Even trace amounts of peanut proteins can trigger an allergic reaction in some people. Therefore, it is essential to avoid foods that may contain peanuts or made in facilities that process peanuts.
Environmental Factors
Environmental factors such as pollution, climate, and living conditions can also contribute to peanut allergy. For instance, children who grew up in urban areas are more likely to develop allergies than those from rural areas. Polluted air can weaken the immune system, making it more sensitive to allergens.
How to Prevent Peanut Allergy
For many years, there has been a great deal of confusion and misunderstanding surrounding peanut allergy, and many people are unaware of how to prevent it. The good news is that there are now many effective ways to prevent peanut allergy from developing
Introduction of Peanuts at an Early Age
Many experts believe that introducing peanuts to babies at an early age can reduce the chances of developing a peanut allergy. Research has shown that children who are exposed to peanuts before the age of six months are less likely to develop an allergy. The introduction should be done carefully and under the supervision of a qualified healthcare professional, ensuring that the child is not already allergic to peanuts.
Exclusive Breastfeeding
Another way to reduce the risk of peanut allergy is by exclusively breastfeeding for the first six months of a baby’s life. Breast milk helps to strengthen a baby’s immune system and reduce the likelihood of developing allergic reactions. If breastfeeding is not possible, certain infant formulas that reduce the risk of food allergies received under the recommendation of a doctor.
Avoid Peanuts during Pregnancy
There is also some evidence to suggest that avoiding peanuts during pregnancy may reduce the risk of peanut allergies in babies. The logic follows that if the mother does not eat peanuts during pregnancy, there will be less chance of exposure to the baby. Health care professionals suggest avoiding peanuts during pregnancy if the mother already has a child with a peanut allergy.
Why Peanut Allergy So Common?
Technological advancements have made it easier to diagnose and track patients with allergies, but the growing trend is undeniable. Experts believe that this rise may be due to several factors, including increased use of antibiotics, a change in the western diet, and more intestinal infections.
Treatment for Peanut Allergy
Medication
When anaphylaxis occurs due to a severe peanut reaction, epinephrine (a synthetic form of the hormone adrenaline) is used to prevent someone from going into anaphylactic shock. People with diagnosed food allergies can be prescribed medications such as EpiPen that automatically inject the medication into the body.
Milder reactions can be treated with antihistamines like Benadryl.
Avoidance
Preventing exposure to peanuts sounds like an obvious and simple solution to peanut allergies, but can be tricky. For one thing, many foods that contain no peanuts are in factories that do handle them. This is when cross-contamination can occur. Second, some foods contain peanut products in ways that aren’t obvious. The importance of reading and understanding food labels cannot be overstated. If there are any questions, contacting the manufacturer is a recommendation.
There is an exception, however. Highly refined peanut oil does not need a label as a peanut ingredient because it has no peanut proteins. Many people with allergies can safely consume it. Keep in mind, though, that this does not apply to cold pressed, expelled or extruded peanut oils. These may contain proteins to which the body can react. “Arachis oil” is another name for peanut oil which may or may not be highly refined.
Biologics
Recently, biologics have emerged as a new treatment avenue for peanut allergy. Biologics are drugs that target specific immune cells or proteins involved in the allergic response. The newest biologic in use for peanut allergies is dupilumab, which reduces inflammation and alleviates symptoms. Studies on the use of this drug for peanut allergy show promise, with nearly half of participants achieving a positive response.
Oral Immunotherapy
While not a cure, oral immunotherapy (OIT) can help make a peanut allergy less dangerous for some people. This experimental technique done in a medical environment involves giving allergic people tiny amounts of peanut in an effort to desensitize the immune system. Successful OIT does not mean a person can begin to eat peanuts. Rather, he or she is less likely to have a life-threatening situation as a result of accidental exposure. Research remains ongoing into the effectiveness and safety of OIT.
Sublingual immunotherapy (SLIT) is another immunotherapy option available for peanut allergy. In SLIT, a peanut allergy extract is under the tongue, and as with OIT, the goal is to desensitize the immune system. However, SLIT involves fewer side effects than OIT, making it a more convenient option for some people.
Other Treatments
Other treatments for peanut allergy include deducing allergic reactions with antihistamines, steroids, and epinephrine, which can treat mild to severe food allergic reactions. Newer treatments such as monoclonal antibodies, which block the IgE antibodies that cause allergic reactions, have also shown promise in clinical studies
Supplements to Help Reduce Allergy Symptoms
Quercetin
Many plant-based foods like blueberries, kale, oranges, turmeric and parsley contain quercetin, which has strong anti-inflammatory properties. Research shows that it can help stop the production of many different types of chemicals in the body that can contribute to allergic responses in people. This applies not only to seasonal allergies, but also food allergies including those to peanuts. It can’t replace medical treatment during a reaction, however. As a supplement, take 250 to 500 mg of quercetin once or twice daily, or as directed by physician.
Butterbur
Butterbur, a plant also known as Petasites hybridus, reduces the body’s production of histamine, the chemical in the body that causes allergic inflammatory reactions. As a result, it can help provide some relief with some of the conditions that co-occur with food allergies like asthma and eczema. Take 150 mg of butterbur extract powder daily with plenty of water or as directed by a physician. The extract powder took for 3-4 months before gradually lowering the dose. If symptoms reappear after lowering the dosage, gradually increase again.
Vitamin C
Vitamin C is a powerful antioxidant that can help reduce inflammation in the body. It’s also a natural antihistamine that can reduce allergy symptoms. Studies have found that taking vitamin C supplements can reduce allergy symptoms like sneezing and runny nose. Vitamin C is in foods like oranges, strawberries, and broccoli, or in supplement form.
Green Tea Extract
Research shows that green tea extract may help to prevent your body from building up an immune response to a range of allergens, which include common ones such as pollen and dust. Green tea naturally contains Epigallocatechin-3-gallate (EGCG), which is believed to be responsible for this anti-inflammatory effect. Green tea extract 50% EGCG is recommended to be taken in servings of 500 mg to be consumed either once or twice a day. Intake should never amount to more than 1,000 mg per day, and this supplement should never be used for more than 3 months at a time.
Stinging Nettle
Stinging nettle is a plant that has been used for centuries to treat allergies. It contains natural antihistamines that can reduce allergy symptoms. Stinging nettle supplements can be found in powder, pill form or in tea form. Taking stinging nettle supplements can help reduce allergy symptoms like sneezing, runny nose, and itchy eyes.
The Bottom Line
In conclusion, peanut allergy treatment options include avoidance, immunotherapy, anti-inflammatory medications, and experimental treatments. It’s essential to consult with an allergist to determine the appropriate treatment plan for managing peanut allergy. Besides, ongoing research is exploring innovative and promising treatment options that may become more widely available in the future. However, regardless of the treatment option chosen, it’s crucial to continue practicing strict avoidance measures to reduce the risk of accidental exposure. With ongoing vigilance and careful management, people with peanut allergy can continue to enjoy a healthy, fulfilling life.
If you’re looking for natural ways to reduce allergy symptoms, supplements can be a great option. Green tea extract, quercetin, vitamin C, butterbur, and stinging nettle are just a few supplements that can reduce allergy symptoms. As with any supplement, it’s important to talk to your doctor before taking them to make sure they’re safe for you. By incorporating these supplements into your diet, you can reduce allergy symptoms and enjoy a better quality of life.
These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure or prevent any disease