What is Cardiomyopathy?
Heart disease remains the leading cause of death in the United States, killing about 630,000 people a year (x). But several major disorders fall under this term. One of these disorders, cardiomyopathy, refers to diseases of the cardiac muscle (the myocardium) which that make pumping blood more difficult. Over time cardiomyopathy causes damage to the heart muscle, loses the ability to pump blood efficiently and leads to chronic heart failure. Cardiomyopathy is also known as congestive heart failure (CHF).
Cardiomyopathy is progressive and incurable. However, treatment can slow it down. This treatment usually consists of prescription medication and lifestyle changes that include a heart-healthy diet and weight loss.
Types of Cardiomyopathy
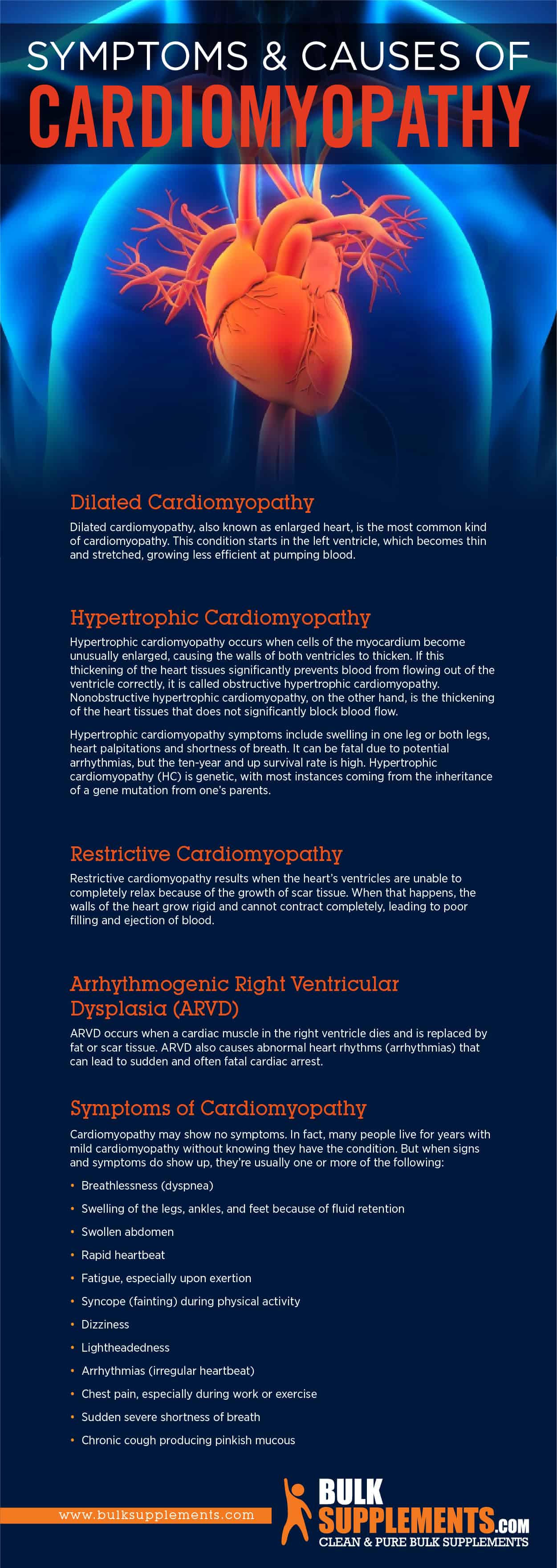
Dilated Cardiomyopathy
Dilated cardiomyopathy, also known as enlarged heart, is the most common kind of cardiomyopathy (x). This condition starts in the left ventricle, which becomes thin and stretched, growing less efficient at pumping blood.
Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy occurs when cells of the myocardium become unusually enlarged, causing the walls of both ventricles to thicken. If this thickening of the heart tissues significantly prevents blood from flowing out of the ventricle correctly, it is called obstructive hypertrophic cardiomyopathy. Nonobstructive hypertrophic cardiomyopathy, on the other hand, is the thickening of the heart tissues that does not significantly block blood flow.
Hypertrophic cardiomyopathy symptoms include swelling in one leg or both legs, heart palpitations and shortness of breath. It can be fatal due to potential arrhythmias, but the ten-year and up survival rate is high. Hypertrophic cardiomyopathy (HC) is genetic, with most instances coming from the inheritance of a gene mutation from one’s parents (x).
Restrictive Cardiomyopathy
Restrictive cardiomyopathy results when the heart’s ventricles are unable to completely relax because of the growth of scar tissue. When that happens, the walls of the heart grow rigid and cannot contract completely, leading to poor filling and ejection of blood (x).
Arrhythmogenic Right Ventricular Dysplasia (ARVD)
ARVD occurs when a cardiac muscle in the right ventricle dies and is replaced by fat or scar tissue. ARVD also causes abnormal heart rhythms (arrhythmias) that can lead to sudden and often fatal cardiac arrest (x).
Symptoms of Cardiomyopathy
Cardiomyopathy may show no symptoms. In fact, many people live for years with mild cardiomyopathy without knowing they have the condition. But when signs and symptoms do show up, they’re usually one or more of the following:
- Breathlessness (dyspnea)
- Swelling of the legs, ankles, and feet because of fluid retention
- Swollen abdomen
- Rapid heartbeat
- Fatigue, especially upon exertion
- Syncope (fainting) during physical activity
- Dizziness
- Lightheadedness
- Arrhythmias (irregular heartbeat)
- Chest pain, especially during work or exercise
- Sudden severe shortness of breath
- Chronic cough producing pinkish mucous
Causes of Cardiomyopathy
Major Causes
The most common cause of dilated cardiomyopathy is severe coronary artery disease or long term coronary artery disease. Coronary artery disease starts when accumulated fatty plaque reduces the levels of fresh oxygen supplied to the heart (x). Increased plaque deposits can also lead to heart attacks, which increases the risk of cardiomyopathy in the future.
Heart attacks, even in the absence of plaque accumulation or arteriosclerosis, can also lead to cardiomyopathy. To illustrate, when a heart attack occurs, the muscle of the heart is deprived of oxygen, causing tissue to die. When muscle tissue dies suddenly, it releases a flood of chemicals into the surrounding areas, causing more damage. In this way, a heart attack causes serious damage to the entire myocardium even if blood oxygen returns rapidly. Once the tissues become weak, cardiomyopathy could result. Not everyone who has a heart attack will develop myopathy.
Other Causes
Causes of enlarged heart include any of the following conditions alone or in combination with other factors.
- Coronary artery disease (arteriosclerosis) — Coronary artery disease is the most common cause of dilated cardiomyopathy (x).
- Chronic high blood pressure — Untreated or poorly controlled high blood pressure is a major contributing factor for cardiomyopathy.
- Chronic rapid heart rate — Tachycardia-induced Cardiomyopathy (TIC) often results from chronic atrial fibrilization, a common heart arrhythmia (x).
- Heart inflammation — Inflammation from diseases like strep can spread to the heart, causing scarring of the heart muscle.
- Iron buildup — Excess iron buildup (hemochromatosis) is hereditary and results from absorbing too much iron from food, but with a lowered rate of iron excretion.
- Substance abuse or addiction — Long-term excessive alcohol abuse, abuse of cocaine, amphetamines, stimulants or anabolic steroids are also contributors (x).
Cardiomyopathy Treatments
While there’s no cure for an enlarged heart, there are ways to slow its progression. In fact, many prescription medications alleviate the symptoms of cardiomyopathy. Some prescription drugs specifically target conditions like high blood pressure and high cholesterol that aggravate cardiomyopathy or otherwise harm the health of the cardiovascular system.
Eating a healthy diet is one of the best ways to help slow the development of cardiomyopathy. Moreover, foods that are dense with nutrients like magnesium, zinc, niacin and vitamins provide daily benefits to your heart. There are also supplements that may help.
Cardiomyopathy Remedies and Supplements
Coenzyme Q10
Coenzyme Q10, also called ubiquinone, is found in every cell of the body and works to prevent damage from oxidative stress. Specifically, Coenzyme Q10 also works within busy muscle tissue to reduce damage from cell processes (x). Take 50mg (about 1/32 tsp) to 200 mg (just under 1/8 tsp) depending on individual needs, or as directed by a physician.
Magnesium
Magnesium helps treat some heart problems, including high blood pressure (x). Take 1,000 mg (1/4 tsp) to 2,200 mg (slightly rounded 1/2 tsp) daily with a meal, or as directed by a physician.
Niacin
Niacin is thought to help cardiac tissue heal, lowers LDL and HDL cholesterol levels and reduce the heart’s susceptibility to stress (x). recommend taking 100 mg (scant 1/16 tsp) to 500 mg (scant 1/4 tsp) daily with meals, or as directed by a physician.
L-Carnitine
L-Carnitine is an amino acid that helps the muscles of the heart use nutrients for energy (x). A dosage of 500 mg once or twice daily is best, unless otherwise directed by your physician.
Vitamin C
Vitamin C has been associated with lowering the risk of coronary artery disease, reducing high blood pressure and has been associated with lowering the risk of coronary artery disease (x).
Omega-3 fish oil
Omega-3 fish oil is associated with dramatic reductions in heart attack and has been demonstrated to reduce triglycerides (x). Try taking 250-500 mg daily, or as directed by a physician.
Alpha Lipoic Acid
Alpha lipoic acid is a protective agent against cardiovascular disease (x). It is one of the most powerful, effective antioxidants known, although it is not as well known as other antioxidants like vitamin E (x). Take 600 mg of ALA one to two times daily, or as directed by a physician.
Medications
There are many medication approaches that can help treat an enlarged heart, such as:
- Angiotensin receptor blockers (ARBs) — ARBs lower blood pressure.
- Angiotensin-converting enzyme (ACE) inhibitors — Lower blood pressure while increasing your heart’s ability to pump blood efficiently, much like ARBs.
- Beta blockers — For improved heart function and lower blood pressure.
- Anticoagulants — Lower your risk of blood clots that might cause a stroke, heart attack or tissue damage in the extremities.
- Anti-arrhythmics — Keep your heart beating without irregular rhythms.
- Diuretics — Flush sodium and excess fluid out of your body, lowering the amount of sodium and water in your tissues. This then reduces blood pressure and helps the heart pump more blood with less force.
Cardiomyopathy Devices, Surgeries and Procedures
There are many medical devices that can regulate a person’s heart rhythm and heartbeat. Here are some of them:
Pacemakers
People with cardiomyopathy benefit from pacemakers that ensure right and left ventricle contractions occur properly (x).
Implantable Cardio-Converter-Defibrillator (ICD)
ICDs are small devices used to treat patients with heart arrhythmias. They are programmed to pick up and stop specific life-threatening arrhythmias – abnormal heart rhythms. An ICD can be a good option for those with severe arrhythmias (x).
Coronary Artery Bypass Graft Surgery (CABG)
CABG surgery uses a vein from the leg or arm to bypass blocked arteries. Your heart may benefit from better blood flow after CABG surgery (x).
Left Ventricular Assist Device (LVAD)
The left ventricle assist device (LVAD), is often called a “bridge-to-a-transplant” is a mechanical pump implanted into the chest that helps the heart pump blood. It helps people who are waiting for a heart transplant survive until they can receive a donor’s heart (x).
Heart transplant
A heart transplant can be an option for people with advanced cardiomyopathy (x).
The Bottom Line
Cardiomyopathy is a common result of coronary artery disease or heart attack. As the heart weakens, it becomes more difficult to pump blood through the body. However, lifestyle changes can slow the progression of the disease or prevent it entirely. There’s good evidence that a healthy diet filled with vital nutrients coupled with exercise can prevent coronary artery disease, thus reducing a person’s chances of developing cardiomyopathy.