You may never have heard of adenomyosis before, but it’s more common than you think. A surprising 20.9 percent of all women may live with it right now. (x) Adenomyosis is a condition that affects the uterus. It is by no means life-threatening and is sometimes hard to diagnose. In fact, many women have it and go about their lives never knowing. (x) (x)
Should this worry you? While adenomyosis is considered benign, it can be excruciatingly painful and severely impact the quality of a patient’s life. Depending on the patient’s age and overall health, it may also adversely affect the ability to conceive. Doctors recommend that patients seek diagnosis and treatment quickly if they are looking to have children. (x) Depending on the symptoms and severity, you can have your adenomyosis treated with surgery or over-the-counter medications. The type of treatment depends partly on the classification, whether focal, focal adenomyoma or diffuse adenomyosis. (x) The most common treatment for older women suffering from severe adenomyosis is a hysterectomy. (x)
What symptoms does adenomyosis cause? How do you tell if it’s adenomyosis or just an irregular period? Should you go to the doctor or just wait it out?
What is Adenomyosis?
What is adenomyosis exactly? Adenomyosis is when the inner lining of the uterus (endometrium) breaks through the inner wall (myometrium) and begins to grow within the uterus lining. The out-of-place endometrial tissue continues with its normal functions: thickening, breaking down and bleeding during the menstrual cycle. But because it’s now in the muscle wall, it causes the surrounding muscles to expand with it. It can cause you severe pain and heavy periods and can impact your fertility. (x) (x)
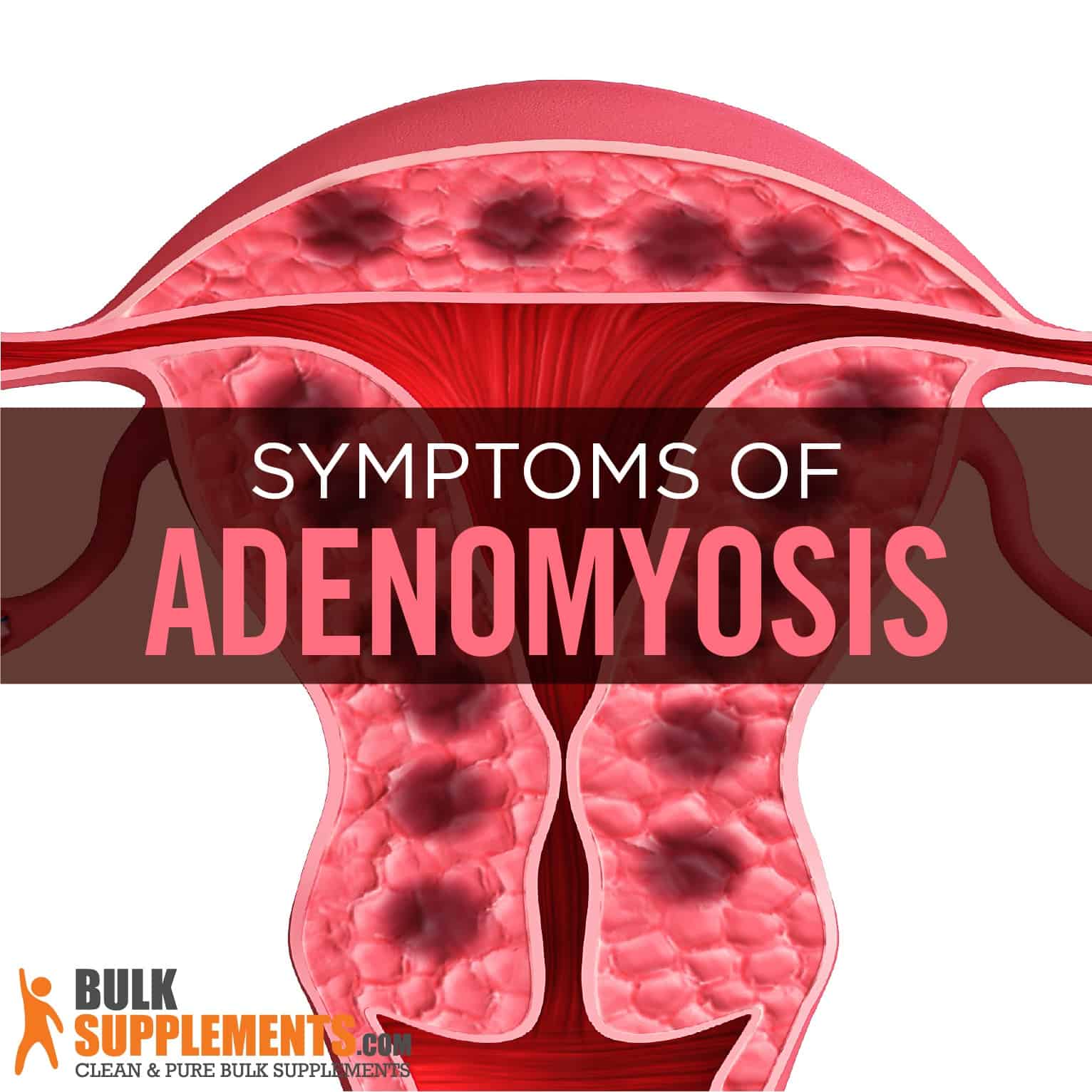
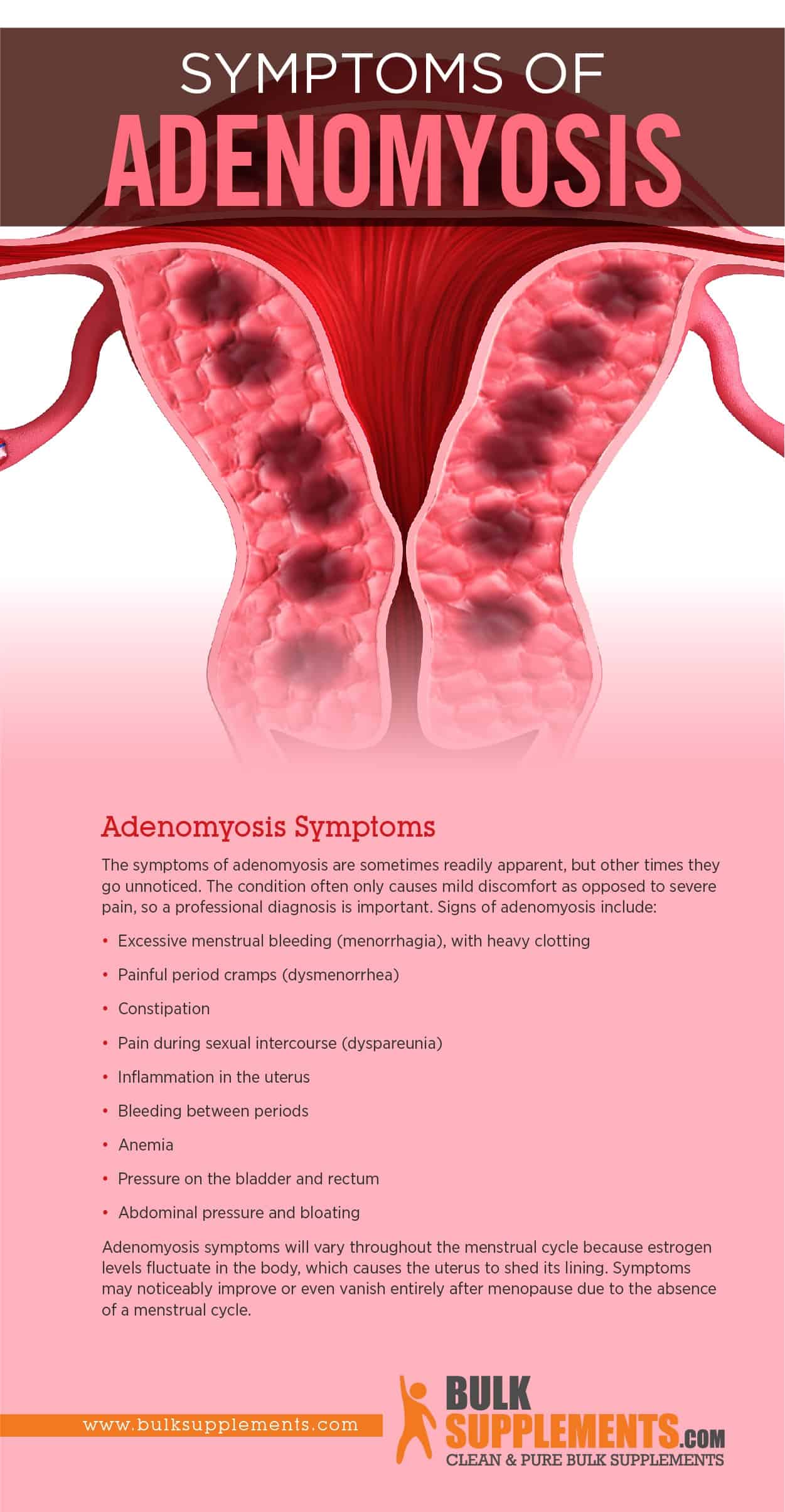
Adenomyosis Symptoms
The symptoms of adenomyosis are sometimes readily apparent, but other times they go unnoticed. The condition often only causes mild discomfort instead of severe pain, so a professional diagnosis is essential. Signs of adenomyosis include: (x)
- Excessive menstrual bleeding (menorrhagia), with heavy clotting
- Painful period cramps (dysmenorrhea) (x)
- Constipation
- Pain during sexual intercourse (dyspareunia) (x)
- Inflammation in the uterus
- Bleeding between periods
- Anemia
- Pressure on the bladder and rectum
- Abdominal pressure and bloating
It’s helpful for you to know that adenomyosis symptoms will vary throughout the menstrual cycle because estrogen levels fluctuate in the body, which causes the uterus to shed its lining. Symptoms may noticeably improve or even vanish entirely after menopause because of the absence of a menstrual cycle. (x)
Adenomyosis vs. Endometriosis
Most women in their lifetime have probably heard of a similar condition called endometriosis. In fact, adenomyosis and endometriosis seem like related conditions. Symptoms can create confusion from one to the other.
So what is endometriosis? It’s a condition where the inner lining of the uterus (endometrium) begins to grow outside of the uterus lining. It can also spread to other parts or organs in the body, like the ovaries and bowels. The fundamental difference between adenomyosis and endometriosis is their location: adenomyosis occurs within the uterus wall, but endometriosis occurs outside of it. (x) (x) (x)
If you experience any of the symptoms listed above, chances are you may have adenomyosis or endometriosis—or even both. It’s possible. For an accurate diagnosis, visit a physician. An MRI or transvaginal ultrasound scans the uterus for signs of either condition. A pelvic exam may also be necessary. (x) (x)
Causes of Adenomyosis
Regardless of the direct cause, the growth of adenomyosis depends on estrogen circulating in the body. When estrogen production declines during menopause, adenomyosis will eventually disappear. Fluctuating hormone levels in the female body may also trigger adenomyosis —estrogen, prolactin, follicle stimulating hormones and progesterone. Physicians do not know the exact cause (or causes) of adenomyosis. However, experts have come up with several theories, many of them related to pregnancy and childbirth. The most common and plausible theories include: (x) (x)
- Invasive Tissue Growth
Some experts believe that invasive tissue growth causes adenomyosis. If you have had any incisions into the uterine wall during operations, such as a C-section. It might cause the endometrial tissue from lining the uterine wall to invade the muscle tissue underneath.
- Stem Cell Origins
The stem cell origins theory is one of the more recent ones. Adenomyosis may develop when bone marrow stem cells invade the uterine muscle. However, because this theory is newer, there are few studies to prove or disprove this idea. (x)
- Developmental Origins
When the fetus first forms in the uterus, endometrial tissue may deposit within the uterine muscle. It may weaken your uterus wall and allow adenomyosis to develop.
- Uterine Inflammation Related to Childbirth
Sometimes during the postpartum period, the uterine lining can become inflamed. It may cause it to weaken and break, allowing the endometrial cells to slip into the uterus wall.
- Vaginal Injury
Vaginal injury may also cause adenomyosis. If the injury causes inflammation, macrophages and cytokines may travel into the myometrium.
Risk Factors for Adenomyosis
According to several factors, some women are more at risk of developing the condition than others. Some include: (x) (x)
- Age
Adenomyosis may develop in all women of reproductive age. However, several studies state that the average woman with adenomyosis is between 32 and 38 years old. (x) Though, the majority are between 40 to 50 years. (x)
- Pregnancy
If you are multiparous, meaning you have given birth more than once, you may be especially at risk of developing adenomyosis. A high percentage of multiparous women have had the condition.
- Uterine Surgery
Uterine surgeries may disturb the endometrial-myometrial border. It may cause the endometrial glands to invade the myometrial layer or muscle wall, leading to adenomyosis.
- Ectopic Pregnancy
Ectopic pregnancy deviates from a normal pregnancy when the embryo attaches itself outside the uterus. It may lead to adenomyosis. (x)
- Antidepressants
Using antidepressants may increase the risk of adenomyosis. These narcotic-type drugs may cause prolactin levels in the body to shoot up, which then over regulates the uterine prolactin receptor messenger RNA, leading to adenomyosis. Prolactin is a hormone that causes milk production during pregnancy, such as lactation and breast enlargement. (x) Fluoxetine, a common psychotropic drug, has terrible effects on women’s reproduction system. An animal study showed the psych drug had a role in causing adenomyosis. (x)
- Breast Cancer
Researchers have identified a connection between postmenopausal women and breast cancer. Patients treated with tamoxifen for cancer and the researchers concluded that adenomyosis was more common in these patients than in those who didn’t receive tamoxifen as a treatment. (x) Tamoxifen is a drug that treats breast cancer when it has spread to other parts of the body — both men and women. (x)
Congruent Disorders of Adenomyosis
Adenomyosis isn’t life-threatening. Still, it’s a cause for concern and may come with complications.
Approximately 40 to 50 percent of patients with adenomyosis may also have endometriosis, which negatively impacts the reproductive system. Adenomyosis patients commonly have decreased fertility or even infertility. Pregnant patients with the disease have a 50 percent miscarriage rate, 24.4 percent preterm birth rate and nearly 12 percent experience a fetal developmental delay. (x) (x)
Fifty percent of patients also develop fibroids, which are non-cancerous tumors that grow on the muscles in the uterus. (x) (x) Patients may also have anemia, a condition where the body has a blood cell deficiency. (x)
Adenomyosis Treatment
Treatment for adenomyosis depends on the severity of the condition. Doctors may also consider other factors like the patient’s health and age. Doctors will classify the type of adenomyosis first and recommend treatments accordingly. Focal adenomyosis and focal adenomyoma do not require a hysterectomy. Diffuse adenomyosis requires a hysterectomy. (x) (x)
There are three primary adenomyosis classifications:
- Focal
Focal adenomyosis is small and “focused” in a single area of the uterus.
- Focal adenomyoma
Adenomyoma is another form of focal adenomyosis. In adenomyoma, a uterine mass or benign tumor may develop in a single section of the uterus.
- Diffuse
Finally, there’s diffuse adenomyosis. Here, the adenomyosis growth spreads throughout the uterus. (x)
Treatments for Adenomyosis
Treatments can be surgical or non-surgical, depending on how the doctor classifies the condition. Some treatments include: (x) (x) (x) (x)
- Medication
A doctor may prescribe medication to treat adenomyosis, some of which also treat endometriosis. Anti-inflammatory drugs may relieve mild pain. Hormonal medications, such as oral contraception, can reduce the symptoms.
- Uterine Artery Embolization
The uterine artery embolization procedure is minimally invasive. Your doctor inserts a tiny tube into an artery in the groin. The tube will transmit tiny particles that block the blood flow to the affected area and reduce the adenomyosis and relieve symptoms.
- Endometrial Ablation
This procedure reduces heavy menstrual bleeding in women by removing a layer from the uterine lining itself. It is limited to patients who do not plan to conceive because they cannot get pregnant after the procedure.
- Laparoscopic Surgery
Laparoscopic surgery or myometrial excision is a minimally invasive technique that treats either focal or adenomyoma adenomyosis. The surgeon removes harmful tissue in the uterus and keeps the uterus intact.
- Hysterectomy
Finally, there is the hysterectomy procedure. Most doctors consider it as a last resort to treat adenomyosis for severe cases classified as diffuse it. The surgeon removes part of the uterus or all of it depending on how the disease has spread.
Hysterectomy Risks & Complications
Hysterectomy is the second most common surgical procedure in women of reproductive age in the United States. Doctors perform approximately 600,000 hysterectomies in the country every year. More than one-third of women in the U.S. have had hysterectomies when they hit 60 years old. (x)
Post surgery, patients may experience infections, hemorrhaging and internal organ damage. The procedure may increase the chance of heart attacks, strokes and early menopause. The process may cause urinary tract infections and increase urination frequency. It may cause depression, decreased sexual sensations, a decrease in lubrication and hormonal deficiencies. After a hysterectomy, a woman can no longer have a biological pregnancy because the procedure removes the uterus. (x)
Supplements for Menstrual Health
Supplements may be a natural option to help promote menstrual health. However, they are not a replacement for medical treatment, and it is best to consult a physician before adding any supplements to your diet.
- Diindolylmethane (DIM)
DIM is an antioxidant that keeps free radicals from causing damage to your body. It may also strengthen the immune system. DIM may help promote menstrual health because it may regulate estrogen levels, which play a role in adenomyosis. It may also help treat premenstrual syndrome (PMS). As a dietary supplement, take 100 to 200 mg once or twice daily or as instructed by a physician.
- Calcium
Even though calcium is the most abundant mineral in the body, the body cannot produce it on its own. It helps promote strong bones and teeth and maintain energy levels. But it may also help with menstruation. A study concluded that calcium supplements might be an effective treatment for mood disorders related to menstruation. (x) The recommended dosage for calcium citrate is 2,380 mg once or twice per day with food unless a physician recommends otherwise.
- Magnesium
Research states that magnesium may be able to help balance menstrual processes. One study tested its effectiveness on PMS symptoms, including depression, insomnia, anxiety, headache and acne. It concluded that the magnesium supplement was more effective than the placebo. (x) Magnesium is present in several different foods, but supplements can help ensure that the body gets enough of it. As a dietary supplement, take magnesium glycinate in 1,600 mg doses once or twice per day with food unless a doctor advises otherwise.
- Ginger Root Extract
Originating in Southeast Asia, ginger is a powerful antioxidant and also has anti-inflammatory properties. It can protect the body from oxidation and inflammation. It is used to treat nausea and indigestion and can potentially reduce menstrual cramps. Research has concluded that it may have a significant effect on relieving your pain, specifically related to menstrual cramps. (x) As a dietary supplement, take 1,000 mg once a day unless a doctor recommends otherwise.
Where to Buy Supplements for Adenomyosis and Menstrual Health?
You can purchase these supplements to help with adenomyosis prevention or treatment at BulkSupplements.com. The company is an industry-leading manufacturer and distributor of pure dietary supplements.
BulkSupplements.com is not just a consumer brand. It also supplies pure ingredients to other food and supplement brands to make their products. All products at BulkSupplements.com are manufactured and tested according to current and proper manufacturing practices.
Are you interested in trying any of these supplements mentioned in this article as a possible solution to helping you with menstrual health and adenomyosis prevention or treatment? Contact BulkSupplements.com to place an order today.
The Bottom Line
Adenomyosis is a common condition in women. Although not life-threatening, the health concern is painful, negatively affects the quality of life and may cause infertility or childbirth issues. It results when the inner lining of the uterus grows toward the uterus muscle. It causes painful period cramps, painful urination and pain during sex.
Some women who have it do not show symptoms. But if they do, a professional diagnosis will classify the type of adenomyosis and plan for appropriate treatment. Medications may treat the symptoms, but patients may require surgery in more severe cases. Supplements can also promote menstrual health, but they are not a replacement for medical treatment. Always consult a physician before implementing new supplements into your diet.
These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure or prevent any disease.