Updated: 11/14/23
Do you suffer from phlebitis, or swelling in the veins? If so, there’s no need to worry. Despite this condition being cardio-vascular related and sometimes painful, it is treatable with a combination of modern medical treatments as well as ingesting certain nutritional supplements. Here, we will discuss how you can make simple lifestyle changes to help relieve your symptoms and elevate your quality of life. Read on for more information about what causes phlebitis and which natural remedies may work best for you!
What Is Phlebitis?
Phleb comes from the Greek word for “vein” and itis refers to inflammation. Therefore, phlebitis simply means “vein inflammation”. Veins run through the entire body, carrying blood away from limbs and organs back to the heart where the blood can pick up more oxygen. When inflamed, a vein can become tender, red, swollen and/or hard.
Phlebitis is a condition that occurs when the lining of a blood vessel gets inflamed. It can occur in any blood vessel in the body but is more commonly seen in the legs. It can be caused by a variety of factors, including injury or trauma, surgery, prolonged sitting or standing, pregnancy, and even cancer. The most common type of phlebitis is superficial phlebitis, which occurs in the veins just below the skin’s surface. It typically manifests as redness, warmth, tenderness, and swelling in the affected area.
Phlebitis can range in severity from mild to life-threatening. It can be superficial, meaning it affects veins close to the skin, or occur in veins located deeper within the body.
The causes of phlebitis vary widely as well. For example, it can arise as a result of a thrombus, or blood clot. In other cases, damage to the vein, reactions to medications, or infections that occur as a result of receiving intravenous injections leads to venous inflammation.
Superficial thrombophlebitis is a type of phlebitis that describes inflammation stemming from a blood clot near the skin. It can be painful but isn’t usually serious. On the other hand, a type of phlebitis called deep vein thrombosis (DVT) can be serious and often requires treatment to prevent life-threatening complications like a pulmonary embolism.
Symptoms of Phlebitis
Phlebitis generally occurs in peripheral areas of the body such as arms and legs. Symptoms around the site of the inflamed vein include (x, x):
Redness
One of the first signs of phlebitis is redness around the affected area. It may start as a small, faint red mark that quickly spreads and becomes more intense. You might feel an uncomfortable burning sensation in this area too.
Swelling
Another symptom of phlebitis is swelling. Your inflamed vein can become swollen, hard, and tender. You may notice your skin becomes shinier in the swollen area, and it might feel hotter to the touch.
Pain
Phlebitis can be incredibly painful, and the intensity may differ according to the location and the extent of inflammation and blood clotting. You can experience pain around the affected area that may also radiate to other surrounding sections.
Warmth
You can also notice warmth in the inflamed area. This is from the increased blood flow to the inflamed area and can be disruptive to your daily routine.
Skin Changes
When phlebitis occurs with blood clotting, the skin can become discolored. The coloration can change from red to dark blue or violet. You may feel that the skin texture is rough, and you might even notice a bulging, cord-like appearance of the veins.
What is Phlebitis of the Leg?
Phlebitis is a condition where the walls of the veins become inflamed, leading to pain, redness, and swelling. One of the most common types of phlebitis is superficial phlebitis, which occurs in the veins just beneath the surface of the skin. This condition is referred to as phlebitis of the leg. While it can occur anywhere in the body, it tends to affect the legs more than any other area.
Complications from Phlebitis
Phlebitis that occurs on surface veins are easy to identify. This isn’t always the case with deep vein thrombosis, however. DVT can go unnoticed until something more serious happens and the blood clot travels to the lungs, known as a pulmonary embolism (PE). The following signs may indicate a PE and require immediate medical attention:
- Trouble breathing
- Rapid heart rate
- Chest pain
- Shortness of breath
- Sweating
- Coughing up blood
- Anxiety
- Lightheadedness
Can Phlebitis Cause a Stroke?
When a vein becomes inflamed, blood flow can be disrupted. This can lead to the formation of blood clots. If a blood clot breaks off and travels to the brain, it can cause a stroke. Research has shown that people with phlebitis are at a higher risk of stroke than those without the condition.
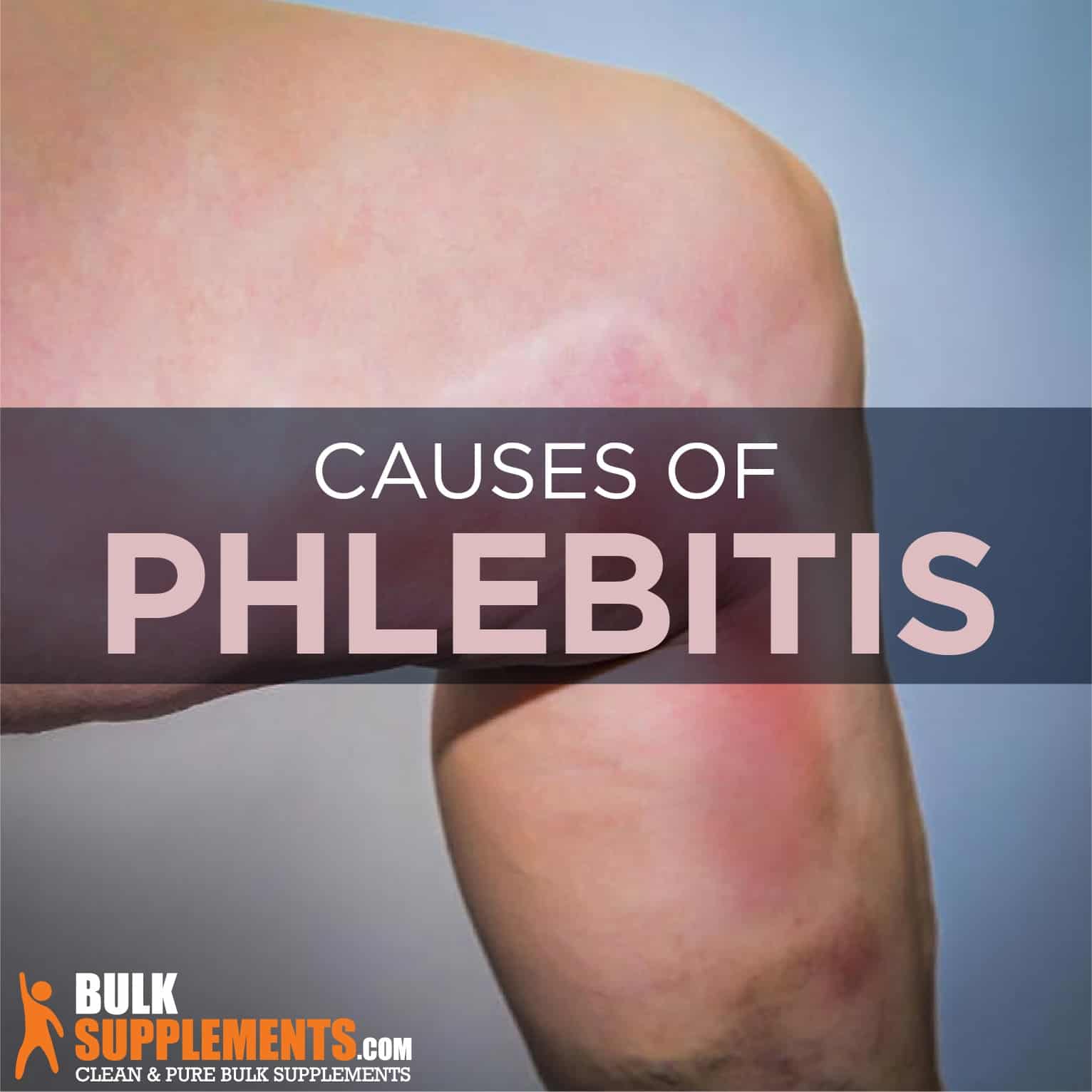
Causes of Phlebitis
Some factors increase the risk of developing phlebitis. We will discuss the main causes of phlebitis that you should know.
Inactivity
Sitting or standing for an extended period without moving can cause phlebitis. Inactivity can lead to poor blood circulation, which can lead to the formation of blood clots in the veins. Long plane or car rides, prolonged bed rest, and sedentary lifestyle are some of the causes of inactivity. To reduce the risk of phlebitis due to inactivity, it is essential to take a break after every few hours of sitting or standing. Stretching or simple exercises can help improve blood circulation.
Injury
Injury to a vein can trigger phlebitis. Wounds sustained during surgery, trauma, or accidents can cause phlebitis. Similarly, inserting an IV line can also cause damage to the vein, leading to phlebitis. The risk of phlebitis due to injuries can be reduced by proper handling of needles during treatments, proper dressing of wounds, and following safety practices when doing physical activities.
Smoking
Smoking is bad for your veins and can cause phlebitis. It can cause your blood vessels to narrow, which can lead to poor circulation in your veins. Poor circulation can lead to blood clots, which can cause phlebitis. If you are a smoker, quitting smoking can significantly reduce your chances of developing phlebitis.
Medications
Some medications increase the risk of developing phlebitis. Estrogen medications, oral contraceptives, and hormone replacement therapy are some of the medications that can cause phlebitis. These medications can cause changes in the blood, leading to the formation of blood clots and inflammation of veins. It is necessary to talk to your doctor about the side effects of medications and ways to manage them.
Chronic Illnesses
Several chronic illnesses increase the risk of phlebitis. Cancer, heart failure, and autoimmune diseases such as lupus can cause inflammation in the veins. These conditions make it difficult for the blood to flow properly, leading to the formation of blood clots. Managing chronic conditions can reduce the risk of phlebitis and other complications.
Genetics
Some individuals have a higher risk of developing phlebitis due to their genetic makeup. Blood clotting disorders such as factor V Leiden mutation and prothrombin gene mutation increase the risk of developing phlebitis. Genetic predisposition to phlebitis can be managed by following a healthy lifestyle, avoiding high-risk activities, and getting regular checkups.
Diagnosing of Phlebitis
The diagnosis of phlebitis can usually be made through a physical examination. The doctor will examine the affected area and check for redness, tenderness, and swelling. They may also order an ultrasound or other imaging tests to confirm the diagnosis and to rule out other possible conditions, such as deep vein thrombosis.
Treatment for Phlebitis
Compression Therapy
One of the most effective treatments for phlebitis is compression therapy. Compression therapy involves wearing compression stockings which help to improve blood flow and reduce inflammation. Compression stockings can be purchased from any health store, and they come in different sizes and styles. Some people also prefer wearing compression bandages, which can soothe the swelling and relieve pain.
Anti-Inflammatory Medications
Another treatment for phlebitis is anti-inflammatory medications. They work to reduce inflammation and relieve pain. Over-the-counter medications such as aspirin, ibuprofen, and naproxen can be used to manage phlebitis. However, always speak to your doctor before using this type of medication, as some people may not be suitable for it.
Hot and Cold Compresses
Hot and cold compresses can also be an effective treatment for phlebitis. Applying heat or cold to the affected area can help to relieve pain and reduce swelling. Ensure that you always use a compress according to the advice of your doctor to avoid worsening the condition.
Muscle Exercises
Gentle exercises can help stimulate blood flow, which can speed up recovery from phlebitis. If you’re experiencing phlebitis, it’s essential to consult your doctor or physical therapist beforehand. They can recommend specific exercises that are not too strenuous and can help you manage the condition.
Surgery
In rare cases, phlebitis may require surgery, especially if further complications such as deep vein thrombosis occur. Surgery may involve the removal of the affected vein or using minimally invasive procedures such as endovenous laser treatment.
Lifestyle Changes
In order to prevent phlebitis from recurring after treatment, it’s important to make some lifestyle changes. This includes maintaining a healthy weight, quitting smoking, and eating a healthy diet. Regular exercise can also help improve circulation in the body, which can help prevent inflammation in the veins. You may also want to elevate your legs when you are sitting or lying down to reduce the pressure on your veins.
Regular Exercise and Healthy Diet
Regular exercise and a healthy diet are vital to treating phlebitis. Exercise boosts blood circulation, preventing blood clots and reducing inflammation. Eating a healthy diet filled with fiber, fruits, and vegetables helps keep our blood vessels healthy and prevent phlebitis.
Vacation
A vacation is always a good idea, but it can also be an effective treatment for phlebitis. Traveling increases the risk of developing blood clots, which can be a severe side effect of phlebitis. Taking a break from your routine and planning a relaxing trip can give you the mental and physical relaxation you need to recover from phlebitis.
Supplements for Phlebitis
If phlebitis concerns you, there are a few ways supplements can help. Some, like turmeric and garlic, have blood-thinning effects. Others, like horse chestnut, can keep the lining of veins strong and prevent swelling. Since some supplements can cause excess bleeding during surgery or interact with other blood thinners, it’s important to consult with your doctor first.
Vitamin E
Vitamin E is a powerful antioxidant that helps reduce inflammation and improve circulation. It also plays a role in reducing blood clots, which can often be a culprit of phlebitis. Studies have found that taking vitamin E supplements can lead to a significant reduction in inflammation and a decrease in pain.
Magnesium
Magnesium is essential for over 300 biochemical reactions in the body, and it also happens to be a natural muscle relaxant. This mineral can help reduce muscle tension and cramps, which can be common symptoms of phlebitis. Taking magnesium supplements can also improve circulation and reduce inflammation.
Omega-3 fatty acids
Omega-3 fatty acids are essential fats that play a crucial role in reducing inflammation and promoting heart health. Taking omega-3 supplements can help reduce inflammation in the body, which can be beneficial for those suffering from phlebitis. You can find omega-3 supplements in the form of fish oil capsules or algae-based supplements for those who are vegetarian or vegan.
Bromelain
This enzyme is found in pineapple stems, and it has great anti-inflammatory properties. Taking bromelain can help reduce swelling, pain, and inflammation in the affected veins. This supplement works by inhibiting the activity of certain enzymes that cause inflammation. It can also break down blood clots and improve circulation. It can be found here in pineapple powder.
Ginger
Ginger has long been used for its anti-inflammatory and antioxidant properties. This supplement can help reduce inflammation and pain in the veins. Ginger can also promote blood circulation, which is essential for maintaining vein health. It can be taken in ginger root extract supplement form or added to food and drinks.
Turmeric Extract
Turmeric is a root similar to ginger. Its active ingredient, curcumin, possesses anti-inflammatory and antioxidant properties. These properties alone help keep veins healthy but curcumin also acts as an anticoagulant, which means it can help prevent blood clots. As a dietary supplement, take 1,000 mg of turmeric root extract daily, or as directed by physician.
Garlic Extract
Garlic is a perennial plant that is known for its sharp taste and distinct aroma. Studies show that healthy consumption of garlic improves well-being and general health. And like turmeric, it also decreases levels of certain proteins in the blood that contribute to clotting. As a dietary supplement, take 650 mg of garlic extract twice daily with meals, or as directed by physician. Be sure to make your discuss with your doctor before surgery.
Horse Chestnut
Studies show that taking horse chestnut can be an effective way to naturally combat a condition called chronic venous insufficiency (CVI). CVI has the potential to cause risk factors related to phlebitis including varicose veins and injury to the vein lining. Therefore, horse chestnut extract can be a useful tool in your arsenal if you’re dealing with inflammation, swelling or discomfort in the legs due to weakened veins. As a dietary supplement, take horse chestnut extract powder 300 mg twice daily, or as directed by physician. Raw horse chestnut is poisonous and should never be consumed raw.
Grape Seed Extract
Not only does grape seed extract help prevent problematic blood clotting, some research shows it helps reduce swelling in the legs caused by poor venous function. Strong veins and blood that flows efficiently reduces the chances of phlebitis. Take 50 mg to 200 mg daily, or every other day, or as directed by physician.
Feverfew Extract
Feverfew is a plant that originated from Asia but can now be found throughout the world. Known to be a naturally occurring stimulant, it contains parthenolides, which assists in the widening of the blood vessels that can provide relief of headaches, migraines and fevers. In addition to that, feverfew may help prevent blood clots and reduce pain and inflammation. The recommended dose for feverfew extract powder is 500 mg to be taken once daily with water or as directed by your medical doctor.
Green Tea Extract
Green tea is rich in polyphenols, plant compounds that operate as antioxidants and neutralize free radicals. Because of this, green tea is well known for overall health-promoting effects ranging from improved skin to cancer prevention (x). It can also help fend off phlebitis by improving the function of veins and protecting them from oxidative damage. As a dietary supplement, green tea extract is recommended to be taken in servings of 500 mg and consumed either once or twice a day.
The Bottom Line
Phlebitis varies in its presentation. Sometimes, like when a person has blood drawn or receives IV fluids through a catheter, a mild case may occur as a result with no consequence. On the other hand, deep vein thrombosis is a potentially deadly form of the condition.
To detect phlebitis, be on the lookout for redness, swelling, warmth, pain, and/or hard bumps under the skin. Unfortunately, the most dangerous type of phlebitis is the hardest to detect because it occurs deep within the body, usually the leg. Should you ever have trouble breathing, changes in heart rate, lightheadedness and any other signs of a pulmonary embolism, seek medical help immediately.
Doctors sometimes prescribe medication to ensure that blood doesn’t clot in the veins. Surgery may also be necessary. In general, staying active and maintaining a healthy weight can keep veins strong and inflammation to a minimum. Finally, plants like turmeric, garlic, feverfew, horse chestnut, and green tea can support blood flow and the proper functioning of veins. Some, like garlic, can easily be built into your diet. Others may be more convenient in the form of supplements. Either way, check with your doctor if you have any questions or if you plan to have surgery in the near future.
These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure or prevent any disease