Updated: 11/6/23
Are you a diabetic? Then you know that it’s important to keep your vision strong, given the risks of developing diabetic retinopathy. This condition can cause vision impairment, and even blindness if left untreated. That’s why we’ve created our range of health supplements specially designed for diabetics! Our unique formula provides a generous amount of essential vitamins and minerals that may help reduce the risk or slow down the progression of diabetic retinopathy. Read on to discover how our supplements could be beneficial for keeping your vision in check!
What is Diabetic Retinopathy?
Diabetic retinopathy occurs when high blood sugar levels damage the tiny blood vessels in the retina, the part of the eye that senses light and sends visual signals to the brain. Over time, these blood vessels become weak and leaky, or they may grow abnormally and form scar tissue. This can cause vision loss or even blindness if left untreated. In fact, diabetic retinopathy is the leading cause of blindness among adults in the United States..
This disease has two stages and while the early stage does not usually cause symptoms, without treatment it progresses into its later stage and the patient suffers more severe symptoms. The condition can even progress to vision loss. Medical researchers report that 7.7 million people in the United States suffer from this disease. Experts further expect this number to reach 14.6 million by 2050.
Two Stages of Diabetic Retinopathy
There are two main stages of diabetic retinopathy: non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR). In its early stages, the condition doesn’t normally show signs and symptoms. But patients usually notice it when the disease starts to progress and when it starts to interfere with vision
Non-Proliferative Diabetic Retinopathy (NPDR)
Many people with diabetes may also have NPDR without realizing it. It causes swelling in the retina and the macula when blood vessels start to leak. NPDR can also cause macular ischemia, which is when the blood vessels in the retina close off. Then, blood flow cannot reach the macula. This can interfere with vision, causing tiny particles to form in the retina.
Proliferative Diabetic Retinopathy (PDR)
NPDR progresses into PDR as the retina grows new blood vessels, a process called neovascularization. But because they are abnormal, the new vessels bleed into the vitreous, the jelly-like substance in the middle of the eye, causing patients to see spots floating in their vision. If the bleeding is heavy, it can cause vision loss and form scar tissue that can cause tears in the retina.
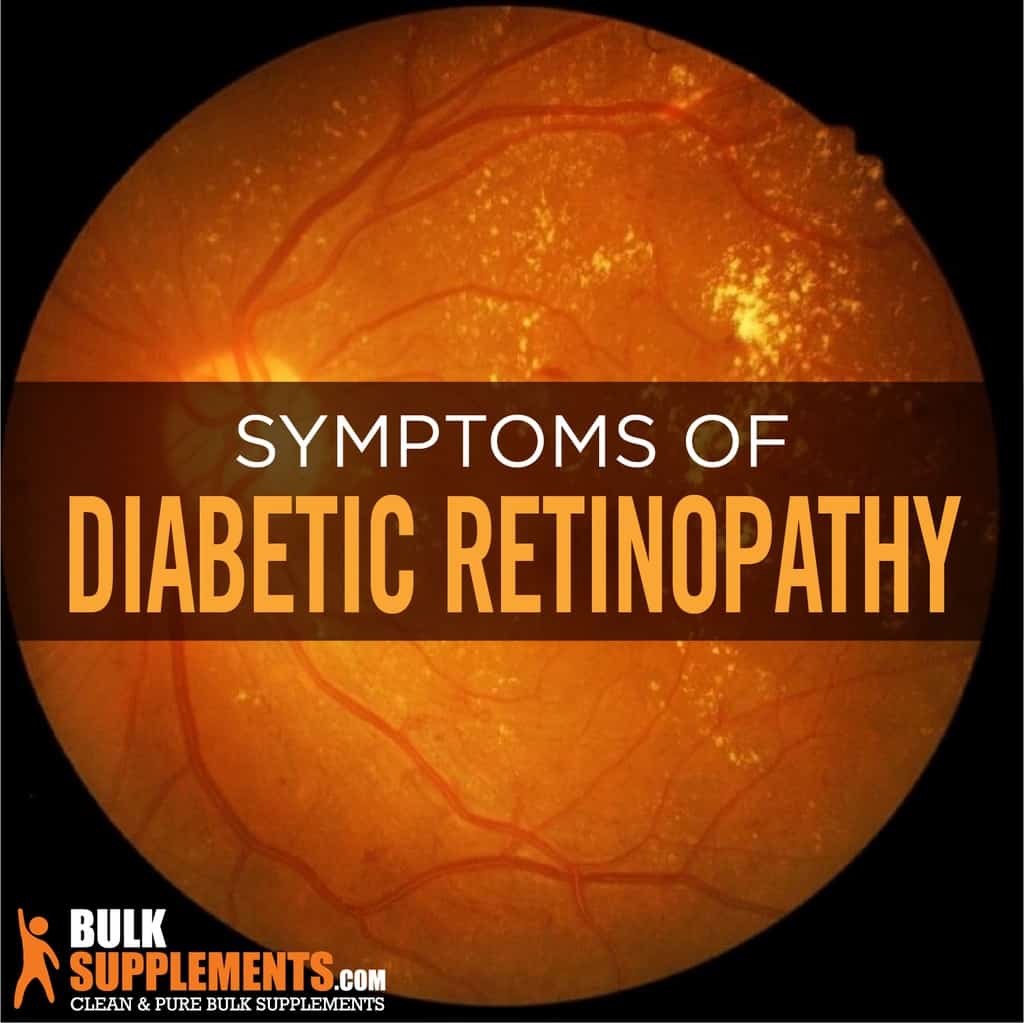
Symptoms of Diabetic Retinopathy
Patients usually begin to notice symptoms in the later stages, compared to the early stage, as they get worse and more noticeable. Symptoms include:
Faded or Washed-out Colors
The first symptom of diabetic retinopathy that you should look out for is faded or washed-out colors. This symptom occurs because the blood vessels in the eyes become damaged. The damage to the blood vessels can cause a lack of oxygen and nutrients to the eyes, which affects your ability to see colors as vibrant as they should be.
Scarring in the Eyes
Scarring in the eyes is another symptom of diabetic retinopathy. The scarring occurs when the blood vessels become damaged and cause fluid to leak into the retina. The retina can start to swell, and the fluid builds up, leading to scarring. This scarring can cause permanent vision loss, so if you notice any scarring, it’s essential to book an appointment with your eye doctor as soon as possible.
Fluid Accumulation
Fluid accumulation is another symptom of diabetic retinopathy. The fluid accumulation occurs when blood vessels become damaged, and fluid starts to leak into the retina. The fluid buildup can cause your vision to become blurry and distorted. The vision may also appear as if you are looking through a smudge or a piece of glass that is dirty.
Sensitivity to Light
Sensitivity to light is another symptom of diabetic retinopathy. It occurs because the blood vessels in the eyes become damaged and leak fluid into the retina. The fluid buildup can cause light to scatter throughout the retina, leading to sensitivity or discomfort when you are exposed to bright lights.
Blurred Vision
What starts as a slight blur can quickly progress over time. This is often the first noticeable symptom you might experience. When diabetic retinopathy causes small blood vessels in the eye to leak, it causes blurred vision. This symptom often comes and goes, and it is more common after eating certain foods, after exercise, or when blood sugar levels are high.
Floaters
Floaters are small spots or specks that drift through your field of vision, often when you are looking at bright scenes. They may appear like cobwebs, tiny dots or birds. These specks are caused by the clumping of cells in the vitreous – the fluid inside the eye – which is responsible for movement. They are not always a symptom of diabetic retinopathy, but if accompanied by other symptoms, seek intervention from an optometrist immediately.
Visual Disturbances
When the level of glucose in your blood remains high, it may cause abnormal, sudden fluctuations in your vision that are often temporary. You may notice flickering lights, black spots, or big floaters.
Eye Pain and Pressure
Diabetic retinopathy often causes high pressure inside the eyes. This could lead to eye pain, redness and discomfort. If you experience sharp pains, headache, or any discomfort in or around the eye, you should get a prompt medical attention to check if it’s related to diabetes or another issue.
Dark Spots in Vision
Another symptom of diabetic retinopathy is dark spots in vision. If you notice black spots in your vision, like darkened or faded patches, it’s essential that you visit your optometrist to rule out retina issues.
Loss of Peripheral Vision
Another symptom of Diabetic Retinopathy is the gradual loss of the peripheral vision. You may not notice this change immediately, but gradually, your vision field gets narrower. Consult an ophthalmologist when it occurs.
Poor Night Vision
If you have diabetes, you may notice that your night vision is not as clear as it once was. This is because the cells in your retina that are responsible for low light vision become damaged over time due to high blood sugar levels. If you struggle to see in low light conditions, even after giving your eyes time to adjust, you may want to discuss this with your eye doctor.
Sudden Vision Loss
In rare cases, diabetic retinopathy can cause sudden and severe vision loss. This can happen if the blood vessels in your retina become completely blocked, preventing blood and oxygen from reaching your eye. If you experience sudden vision loss, seek medical attention immediately.
How Does Diabetes Cause Retinopathy?
How does diabetes cause retinopathy? The answer is due to high blood sugar levels. When you have diabetes, your body cannot produce or use insulin properly. As a result, your blood sugar levels rise, which can damage blood vessels and nerves throughout your body, including those in your eyes. Over time, this ongoing damage can cause the blood vessels in your retina to weaken, leak, or even close off.
Causes of Diabetic Retinopathy
Diabetic retinopathy is a complication from diabetes, which interferes with how the body uses and stores glucose. Patients have too much sugar in their blood and it causes damage to the blood vessels, including the ones in the eyes. The blood vessels can leak blood and fluid that builds up in the retina, causing swelling and changes in vision. When fluid accumulates in the retina, it can make it difficult for the eyes to focus, resulting in cloudy or blurry vision. It is important to understand the causes of diabetic retinopathy and know the steps to take to prevent it from developing.
Poor Blood Sugar Management
One of the primary causes of diabetic retinopathy is high blood sugar levels which can damage the blood vessels in the retina, leading to vision problems. Poor blood sugar management can also trigger the production of new blood vessels that are fragile and prone to leaking into the retina, causing vision loss. This is why it’s crucial for people with diabetes to maintain a healthy blood sugar level to prevent the onset and progression of diabetic retinopathy.
High Blood Pressure
People with diabetes also face an increased risk of developing high blood pressure, which can contribute to the progression of diabetic retinopathy. High blood pressure decreases the oxygen supply to the retina, leading to vision problems. It can also cause damage to the blood vessels in the retina, amplifying the progression of diabetic retinopathy. It’s important to get your blood pressure checked regularly and take medications if deemed necessary by your doctor.
High Cholesterol Levels
High levels of LDL or “bad” cholesterol can lead to plaque buildup on the walls of your arteries, including those that nourish your eyes. This can affect the blood supply to the retina, leading to vision problems. Maintaining healthy cholesterol levels via a balanced diet of whole grains, fruits, and vegetables, and avoiding high-fat foods can reduce the risk of developing diabetic retinopathy.
Length of Time You Have Had Diabetes
The duration of time you have diabetes is a contributing factor to the development of diabetic retinopathy. The longer you have had diabetes, the higher the risk of developing retinopathy. Regular checkups with your doctor like A1C tests can help to monitor your blood sugar levels and reduce your risk of developing this silent disease.
Smoking
Smoking damages the blood vessels, increasing the progression and severity of diabetic retinopathy. In fact, smokers with diabetes have three times the risk of developing the condition than non-smokers. If you smoke, quitting is the best thing you can do for your health. It’s never too late to quit smoking, and your doctor can help you come up with a plan.
Genetics
The risk of developing diabetic retinopathy also depends on one’s genetics. If you have a family history of diabetes or diabetic retinopathy, you should take extra precautions to maintain a healthy lifestyle and blood sugar control, as your genetics may amplify your risk of developing the condition.
How Diabetic Retinopathy is Diagnosed
Many patients with diabetes already have diabetic retinopathy without even realizing it. However, it is important for patients to see an ophthalmologist regularly, even if they do not notice any symptoms. It is equally important to visit a doctor for an exam if the patient does start to notice changes in their vision. Diabetic retinopathy is a serious complication from diabetes that can cause blindness without treatment.
There are several ways to diagnose this condition and look for abnormal blood vessel growth in the retina, bleeding in the vitreous, retinal detachment or swelling in the retina. The doctor may dilate the eyes with drops to widen them. The ophthalmologist will use a special lens to examine the inside of the eye. The doctor may also use a fluorescein angiography or optical coherence tomography to examine the eye. Fluorescein is a yellow dye that the doctor injects into a vein and uses a camera to take photos of the retina as the dye flows through the blood. On the other hand, optical coherence tomography uses a machine to scan the retina and detect swelling.
Can Diabetic Retinopathy Be Reversed?
Unfortunately, diabetic retinopathy cannot be reversed. However, early detection and proper management can prevent it from worsening and causing further damage to the eyes. That is why it is essential to get yearly eye exams to detect any changes in the eyes.
Can Diabetic Retinopathy Be Treated?
Diabetic retinopathy is a severe complication of diabetes that can potentially lead to blindness if not appropriately treated. However, with early detection and proper management, diabetic retinopathy can be treated effectively. Treatment options range from laser treatment to eye injections and surgical procedures. Working with your healthcare provider and an eye specialist can help you get the best treatment possible. If you’re experiencing symptoms related to diabetic retinopathy, don’t wait – early detection and treatment are crucial to improving your eyesight and preventing further complications.
Treatment for Diabetic Retinopathy
There are different treatment options for this condition depending on how it affects the patient’s eyes. It’s important to seek treatment as soon as possible to preserve vision and avoid complications.
Regular Eye Exams
The most effective way to prevent or treat diabetic retinopathy is to have regular eye exams. This allows your eye doctor to detect any changes in your eyes before they become more serious. If you have diabetes, it is recommended that you have a dilated eye exam at least once a year. This will also help to ensure that you receive the appropriate treatment for your condition.
Laser Treatment
This is the most common form of treatment for diabetic retinopathy. Lasers are used to seal leaking blood vessels in the retina, which prevents further damage to the eye. The procedure is painless and takes only a few minutes to complete. You may experience some discomfort during the procedure, but it is generally well-tolerated. In some cases, multiple sessions of laser treatment may be required to achieve the desired results.
Anti-VEGF Injections
These injections are given directly into the eye to block the growth of new blood vessels in the retina. This treatment is often used in conjunction with laser treatment to achieve the best results. You may need to receive injections on a regular basis to maintain the effectiveness of the treatment.
Vitrectomy
This is a surgical procedure that is used to remove the vitreous gel in the eye. This gel can become cloudy due to bleeding from damaged blood vessels in the retina. By removing the gel and replacing it with a clear solution, your vision can be restored. This procedure is usually reserved for more advanced cases of diabetic retinopathy.
Lifestyle Changes
In addition to medical treatment, making changes to your lifestyle can help to prevent or slow down the progression of diabetic retinopathy. Maintaining a healthy weight, exercising regularly, and controlling your blood sugar levels are all important factors in maintaining good eye health. Quitting smoking is also essential, as smoking can increase your risk of developing diabetic retinopathy.
Living with Diabetic Retinopathy
Preventing Vision Loss
The best way to prevent vision loss is to get prompt treatment. Doctors may detect the condition before it even causes symptoms, so it’s important to get regular eye exams. If there are symptoms, seek medical attention as soon as possible. Patients with diabetes should take care about controlling the condition to avoid diabetic retinopathy as a complication. High blood pressure damages blood vessels all over the body including the eyes.
Diet
Since diabetic retinopathy is a result of diabetes, there may be a connection between it and dietary choices, which also plays a role in diabetes. In one study, researchers concluded that a Mediterranean diet and low calorie intake may reduce the risk. Patients should control their blood sugar, blood pressure and cholesterol with healthy dietary habits. Maintain a consistent diet of healthy carbs, increase fruit and vegetable intake and limit sodium and alcohol. Foods rich in beta-carotene and vitamin A may help preserve vision, such as pumpkin, papaya, oranges, kiwis, sweet potatoes, carrots, leafy green vegetables, eggs and fish. The more color in a fruit or vegetable, the more beta-carotene it contains.
Supplements for Diabetic Retinopathy
In addition to lifestyle practices and medical treatment, patients may also help control the condition with natural compounds and nutrients. Supplements are a good way to stay healthy, but it’s important to consult a doctor for approval before starting a regimen. They are not a cure or a complete prevention for any medical condition, but they may be able to boost in overall health.
Vitamin A
Vitamin A has two different categories, carotenoids and retinoids. Both of them exist in food, but the body can absorb retinoids easier, so they are more common in dietary supplements. Vitamin A is an antioxidant that can help reduce free radicals, unbalanced molecules that cause damage and disrupt body systems. It is a common treatment for illnesses, skin conditions and eye health. Research suggests that vitamin A may be able to improve vision and help treat several different eye diseases. It is present in various foods, but patients can also take vitamin A palmitate powder as a supplement for a consistent dosage. The recommended serving is 30 mg daily, unless a doctor recommends a different dosage.
Vitamin E
Vitamin E is a group of fat-soluble antioxidant compounds. Like vitamin A, it can help neutralize free radicals and fight disease, such as cancer or heart disease. Vitamin E deficiency can damage the immune system, weak muscles, neuron degeneration and even retinopathy. Research studies have produced evidence that vitamin E may reduce the risk of age-related vision problems, with the help of vitamin C, zinc and beta-carotene. As a dietary supplement, the recommended dosage for vitamin E powder is 500 to 1,000 mg (about ¼ to ⅓ tsp) daily, if a doctor approves the dosage.
Omega-3 Fatty Acids
Omega-3 fatty acids, found in fish oil supplements, have been shown to significantly reduce the risk of diabetic retinopathy. These acids help to reduce inflammation, which is known to contribute to the development of the condition. Taking fish oil supplements helps to regulate blood sugar levels and prevent the narrowing and clotting of blood vessels, thus supporting the health of the eyes.
Lutein and Zeaxanthin
These carotenoids are found in green leafy vegetables such as kale and spinach, but can also be taken as dietary supplements. They contain antioxidants that protect the eyes from free radicals and reduce the risk of age-related eye disorders such as macular degeneration, cataracts, and diabetic retinopathy. Studies have also shown that lutein and zeaxanthin supplements improve visual function and protect the eyes from harmful blue light.
Beta-Carotene
Beta-carotene is a carotenoid, a plant pigment in fruits, vegetables, herbs and spices. The body converts into vitamin A, but it can also improve health on its own. It can help support the reproductive system, immune system and respiratory system. Beta-carotene also promotes eye health and studies claim that it may be able to reduce the progression of age-related macular degeneration, which is a major factor in adult blindness. As a dietary supplement, the recommended dosage for beta-carotene 1% (CWS) powder is 1,300 mg (about ½ tsp) daily, after consulting a doctor.
Ginkgo Biloba
Ginkgo biloba is a common ingredient in natural medicine practices and health supplements. It is rich in antioxidants and may help fight diseases related to oxidative stress, like inflammatory diseases, Parkinson’s disease and Alzheimer’s disease. Hypertension is also related to oxidative stress and can cause diabetic retinopathy. It may also help with eye diseases specifically, such as glaucoma. The recommended dosage for ginkgo biloba leaf extract powder is 175 mg two or three times a day, or following a doctor’s instructions.
Astragalus
Astragalus is a plant genus with more than 2,000 species, mostly herbs and small shrubs that grow in temperate climates in the Northern Hemisphere. It is a common ingredient in herbal medicine practices in China and Persia. Astragalus supports immune health, cardiovascular health and liver function. It may also help patients suffering from heart disease, arthritis and high blood pressure. The recommended daily dosage for astragalus extract powder is 1,300 milligrams a day. Take the supplement with food and make sure to consult a doctor before adding it to a dietary regimen.
Zinc
Zinc is an essential mineral that helps the body regulate its immune system and repair damaged tissues. Diabetic retinopathy damages the blood vessels in the eye, and taking zinc supplements can help to repair these delicate blood vessels. Zinc also has antioxidant properties that protect the eyes from free radical damage.
Chromium
Chromium helps to regulate blood sugar levels. This mineral has been shown to improve glucose tolerance and reduce insulin resistance in people with type 2 diabetes. By helping to regulate blood sugar levels, taking chromium supplements can help to prevent the progression of diabetic retinopathy.
Alpha-Lipoic Acid
Alpha-lipoic acid is a potent antioxidant that can help to prevent damage to the blood vessels in the retina. It works by reducing oxidative stress, which is a significant risk factor for diabetic retinopathy. Studies have shown that taking alpha-lipoic acid supplements can reduce the progression of diabetic retinopathy by up to 75%. It is found in foods such as spinach, broccoli, and liver, but the best way to get enough of this nutrient is by taking a supplement.
The Bottom Line
Diabetic retinopathy is a complication from diabetes, which damages blood vessels throughout the body. It can also damage the blood vessels in the retina and interfere with vision. Symptoms include blurry or cloudy vision, fluid accumulation, scarring and sensitivity to light. Without treatment, patients can lose their eyesight completely. Treatment options include medication to reduce swelling, laser surgery to shrink the blood vessels and vitrectomy to remove fluid, blood vessels or scar tissue from the eyes. Managing blood pressure and blood sugar can also help manage the condition and possibly even reverse vision damage.
Supplements for Diabetic Retinopathy are an effective way to protect your eyesight naturally. These supplements work by providing essential nutrients that help to reduce inflammation, prevent oxidative stress, and improve blood flow to the eyes. Omega-3 fatty acids, Vitamin C, Vitamin E, Zinc, and Alpha-Lipoic Acid are some of the best supplements to take to prevent and treat diabetic retinopathy. However, it is essential to consult with your physician before beginning any supplement regimen, as some supplements can interact with medications you may be taking. With proper care, you can manage your diabetic retinopathy and protect your vision for years to come.
These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure or prevent any disease