Updated: 9/22/23
The pancreas is an important organ in the human body, responsible for the production of digestive enzymes and hormones such as insulin. However, when the pancreas becomes inflamed, a condition called pancreatitis occurs, which can cause significant damage to the body if left untreated. In this blog post, we will discuss the symptoms, causes, and treatment options for pancreatitis.
What is Pancreatitis?
The suffix “itis” references inflammation and is often attached to a number of medical conditions that humans face. Much like this term implies, pancreatitis refers to inflammation of the pancreas and can have a large number of causes. These causes may be either acute or chronic and depend on many factors including lifestyle, genetics, diet and more.
To understand just how the inflammation of the pancreas affects the human body, it is important to understand the role that the pancreas plays within the digestive system. As an organ located in the upper abdominal region, it primarily serves in the capacity of two vital functions, listed below:
- The first function is to release enzymes into the digestive tract. These enzymes have the ability to help break down food, release necessary nutrients into the body and prepare waste products for excretion after further filtering.
- The second function is to release the hormone “insulin.” The purpose of this hormone is to help regulate blood glucose levels. This ensures that individuals’ blood sugar is maintained in a healthy range, avoiding diabetic ketoacidosis, diabetic coma and more.
When the pancreas becomes inflamed, it often is the result of lack of proper function. This causes a lack of regulation within the digestive tract. It may also cause issues with digestion of food or lack of regulation of blood glucose levels, thus leading to diabetes and secondary conditions.
Pancreatitis Symptoms
It may be confusing to understand abdominal symptoms and how to differentiate among a number of conditions based on the symptoms. However, pancreatitis does have a unique presentation that can help rule out a number of other conditions.
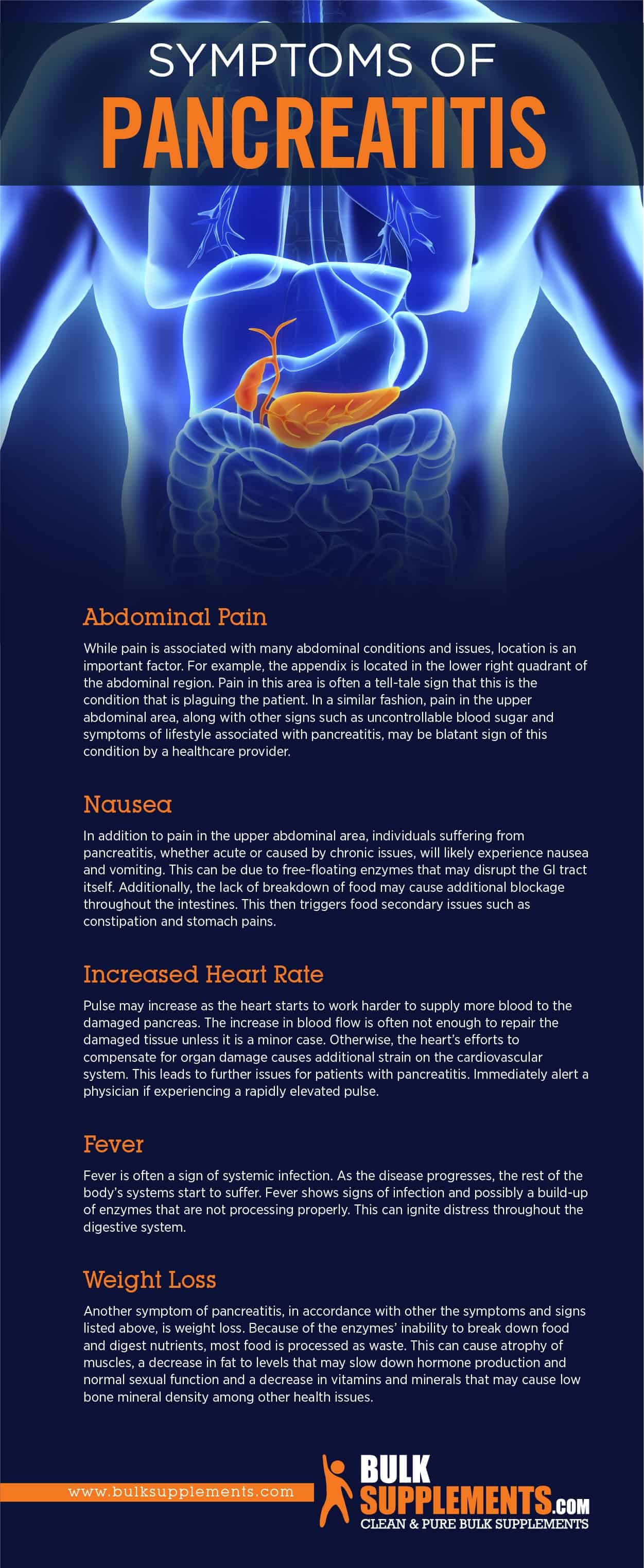
Abdominal Pain
While pain is associated with many abdominal conditions and issues, location is an important factor. For example, the appendix is located in the lower right quadrant of the abdominal region. Pain in this area is often a tell-tale sign that this is the condition that is plaguing the patient. In a similar fashion, pain in the upper abdominal area, along with other signs such as uncontrollable blood sugar and symptoms of lifestyle associated with pancreatitis, may be blatant signs of this condition. If you experience severe abdominal pain that does not go away after a few hours, seek medical attention immediately.
Nausea
In addition to pain in the upper abdominal area, individuals suffering from pancreatitis, whether acute or caused by chronic issues, will likely experience nausea and vomiting. This can be due to free-floating enzymes that may disrupt the GI tract itself. Additionally, the lack of breakdown of food may cause additional blockage throughout the intestines. This then triggers food secondary issues such as constipation and stomach pains. In some cases, the nausea may be severe enough to prevent you from eating or drinking, which can lead to dehydration. If you experience persistent nausea and vomiting, you should consult your doctor.
Jaundice
Jaundice is another common symptom of pancreatitis. It is caused by the buildup of bilirubin in the blood, a yellow pigment produced by the liver. Jaundice can cause yellowing of the skin and eyes, dark urine, and itchy skin. It can indicate that the pancreatitis is severe and requires immediate medical attention.
Increased Heart Rate
Pulse may increase as the heart starts to work harder to supply more blood to the damaged pancreas. The increase in blood flow is often not enough to repair the damaged tissue unless it is a minor case. Otherwise, the heart’s efforts to compensate for organ damage causes additional strain on the cardiovascular system. This leads to further issues for patients with pancreatitis. Immediately alert a physician if experiencing a rapidly elevated pulse.
Fever
Fever is often a sign of systemic infection. As the disease progresses, the rest of the body’s systems start to suffer. Fever shows signs of infection and possibly a build-up of enzymes that are not processing properly. This can ignite distress throughout the digestive system.
Weight Loss
Another symptom of pancreatitis, in accordance with the other symptoms and signs listed above, is weight loss. Because of the enzymes’ inability to break down food and digest nutrients, most food is processed as waste. This can cause atrophy of muscles, a decrease in fat to levels that may slow down hormone production and normal sexual function and a decrease in vitamins and minerals that may cause low bone mineral density among other health issues.
Are Pancreatic Cysts Cancerous?
If you or someone you know has been diagnosed with a pancreatic cyst, you are probably wondering whether it is cancerous. The answer isn’t always straightforward. The truth is that it might be. With the right information and knowledge, we can better understand and manage pancreatic cysts.
Are Pancreatic Cysts Common?
Pancreatic cysts are abnormal pocket-like formations filled with fluid found in the pancreas. These cysts can be either benign or cancerous, and their prevalence has been steadily increasing over the years. If you are wondering if pancreatic cysts are common, the answer is yes. However, not all of them are harmful.
Pancreatitis Causes
As stated, there are many causes than can lead to developing pancreatitis. Some of these causes are acute and others are chronic in nature. The following have a common connection to pancreatitis.
Gallstones
One of the most common causes of pancreatitis is gallstones. When these stones form, they can get stuck in the duct that connects the pancreas to the common bile duct, which in turn, causes inflammation. While gallstones aren’t always preventable, you can reduce your risk by maintaining a healthy weight, eating a balanced diet, and staying physically active. If you’re experiencing symptoms like abdominal pain, nausea, and vomiting, it’s essential to see a doctor and get checked for gallstones.
Genetics
Individuals with a family history of pancreatitis are more likely to develop the condition themselves. There are genetic factors that increase the risk of developing the disease, particularly mutations in the cystic fibrosis gene. Screening tests are available for individuals with a family history of pancreatitis to check for any genetic mutations.
Cystic Fibrosis
Another common cause for the disease in a chronic nature is the diagnosis of cystic fibrosis. As cystic fibrosis causes lesions in the pancreatic ducts in which enzymes flow, the enzymes are blocked and are unable to maintain normal function. This results in chronic inflammation of the pancreas as it struggles to maintain its role in the GI tract.
Infection
A general infection may also cause pancreatitis acutely. Normally, infection may spread and can engage the pancreas, at which point regular function will start to break down (x). In some cases, the pancreas can become infected by bacteria or viruses, causing inflammation and other symptoms. Taking steps to prevent infections, such as practicing good hygiene and avoiding contact with people who are sick, can help reduce your risk of developing pancreatitis.
Alcoholism
Alcoholism is another common cause for pancreatitis. Alcohol is rich in sugars. For those who are drinking constantly, the pancreas must work hard to produce insulin in order to balance out these sugars and maintain healthy blood glucose levels. As the pancreas must work excessively to keep these levels within a normal and healthy biologic range, it can easily become overworked and start to break down. Once this breakdown begins, continued usage of alcohol in excess continues to stress the organ, causing further damage. For many alcoholics with this condition, the only remedy is invasive surgical procedures in addition to major lifestyle changes.
Trauma
Physical injury to the pancreas or surrounding organs can cause an acute form of pancreatitis. For instance, a punch to the abdomen or a car accident could result in pancreatitis. It’s vital to seek medical attention immediately if you suffer any trauma that targets the upper abdomen.
Can Pancreatitis be Cured?
While there is no cure for pancreatitis, managing the condition can help prevent complications and improve quality of life. Lifestyle changes, such as quitting smoking, reducing alcohol consumption, and eating a low-fat diet, can help manage symptoms of pancreatitis and prevent further damage to the pancreas. Medications to manage pain, improve digestion, and control blood sugar levels.
Pancreatitis Treatment
Pain management
The pain associated with pancreatitis can be severe and debilitating. Pain management is an essential part of treating pancreatitis and can involve a range of medications, such as painkillers and anti-inflammatory drugs. Some people may also benefit from alternative treatments such as acupuncture, massage therapy, and relaxation techniques.
Nutritional Changes
Nutritional changes are an important aspect of pancreatitis treatment. The goal is to reduce the amount of stress on the pancreas by making changes to your diet. This may include avoiding alcohol and fatty or fried foods, and instead opting for a diet rich in lean protein, fruits, and vegetables. In some cases, a liquid diet flows to the pancreas time to heal.
Enzyme Replacement Therapy
In some cases, pancreatitis can cause damage to the pancreas, which can affect its ability to produce digestive enzymes. Enzyme replacement therapy can help to manage this issue by providing the necessary digestive enzymes to the body. This therapy administers through oral medication or injections.
Endoscopic Procedures
Endoscopic procedures treat pancreatitis by gallstones or other blockages in the pancreas or bile ducts. During an endoscopic procedure, a small camera inserts into the mouth and guides down into the digestive system. From there, the physician can make incisions and remove any blockages, as well as take tissue samples for analysis.
Hospitalization
In severe cases of pancreatitis, hospitalization may be necessary. During hospitalization, the patient receives intravenous fluids and nutrition to help the pancreas heal and manage the symptoms. In some cases, surgery may also be necessary to remove damaged tissue around the pancreas. For severe cases of pancreatitis, surgery may be necessary. This is particularly true if the pancreas has an infection or if there is a large amount of dead tissue that needs to be removed. The most common surgical procedure for pancreatitis is a pancreaticoduodenectomy (Whipple procedure).
Are Pancreas Transplants Possible?
A pancreas transplant involves removing a healthy pancreas from a deceased donor and transplanting it into a recipient with a diseased or damaged pancreas. The surgery can be performed alone or together with a kidney transplant, as many people with pancreatic diseases also suffer from kidney failure due to complications of diabetes or other conditions. The success rate of pancreas transplant varies depending on several factors, such as the age and overall health status of the recipient, the quality of the donor pancreas, the skill of the surgical team, and the post-transplant care and surveillance.
Pancreatic Remedies and Supplements
There are many invasive procedures and medications available for severe cases of pancreatitis. However, there are also a number of natural remedies available for minor cases. While each course of treatment should be individualized and discussed with a physician, the following remedies have all been used to different degrees of success for many patients suffering from pancreatitis:
Rhodiola
Rhodiola is a natural herb that has a wide array of uses. It may aid the immune system response to bodily stresses that have systemic implications. When a patient suffers from pancreatitis, the immune system kicks into overdrive as it attempts to respond to the damage to the organ. Aiding this system helps to create improved bodily defense to infection. Rhodiola rosea can assist with healing, especially in moderate cases of pancreatitis.
Reishi Mushroom
Reishi mushroom is a naturally grown herb offers a wide array of uses for different conditions throughout the human body. Commonly, it gears to aiding the immune system. In addition, this herb is a known anti-inflammatory that possesses the ability to work systemically. While many anti-inflammatories work primarily in fighting mild muscle and joint inflammation, reishi mushrooms can help the GI tract and organs in other vital parts of the body. Supplementing with this herb may help reduce symptoms as well as lower the amount of damage done by the disease.
Glutamine
Glutamine is an amino acid that serves a wide array of functions. As an amino acid, it is a building block of protein and assists with bodily recovery and growth. However, it additionally serves an added role in intestinal health within the GI tract. When damage happens to the pancreas, tissue breakdown occurs. Glutamine is geared towards specifically assisting with the recovery of epithelial tissue as needed within the GI tract. This supplementation may be ideal for those rebounding from an acute bout of pancreatitis. It also provides benefits to those suffering from chronic illnesses.
Coconut Oil
Coconut oil is a great anti-inflammatory that has possible systemic benefits for those with a wide array of illnesses. As it works in this capacity, it can possess the ability to reduce conditions that affect the GI tract. It is for symptom alleviation for those suffering from chronic pancreatitis.
Acupuncture
Acupuncture works along the lines of assisting with meridian pain and pathology. With proper acupuncture, many believe that they can help to minimize pathology, such as pancreatitis and other inflammatory responses.
Yoga
While this treatment has had varying degrees of results, a great number of pancreatitis patients have seen profound benefits from the regular implementation of yoga. The idea behind this remedy is to relieve stress within the body. Stress can have significant effects on the GI tract and cause inflammation. Only partake in yoga when under the supervision of a professional.
The Bottom Line
Pancreatitis can be a very troubling condition with many secondary systemic effects. For those suffering from diabetes, this is an issue that should be addressed immediately in order to ensure the right remedies and treatment options are available. While many cases can be solved through natural remedies and minimal intervention, the best course of treatment needs to have a discussion with a physician to ensure all necessary steps are taken.
Pancreatitis treatment is a complex and ongoing process that requires a multidisciplinary approach. It is essential to work closely with a healthcare provider to develop an effective treatment plan that addresses your individual needs. By making lifestyle changes, managing underlying conditions, and seeking medical attention as soon as possible, you can effectively manage your pancreatitis and improve your overall health and well-being. If you experience any symptoms of pancreatitis, speak to your healthcare provider immediately. Early diagnosis and treatment can make a significant difference in managing this condition.
These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure or prevent any disease