What is Narcolepsy?
Narcolepsy is a chronic neurological disorder that results from the body’s inability to regulate sleep cycles. It is a rare medical condition estimated to occur in 1 out of 2,000 individuals. (x) Narcolepsy can cause severe disruptions to a person’s daily activities. Most individuals with this condition have trouble falling asleep at night and experience daytime sleepiness. Many people experience uneven and interrupted sleep and uncontrollable, intermittent episodes of falling asleep throughout the day. (x)
Types of Narcolepsy
There are two common types of narcolepsy: (x) (x) (x)
Narcolepsy Type 1
This type shows excessive daytime sleepiness, combined with either low levels of hypocretin (help regulate sleep patterns), characteristics of cataplexy or both. Cataplexy causes a sudden loss of muscle tone while you’re awake, such as slurred speech or even paralysis.
Narcolepsy Type 2
This type does not include cataplexy. Patients feel excessively tired during the day but do not have muscle weakness or paralysis. The symptoms are less severe, and hypocretin levels are not as irregular.
Secondary Narcolepsy
People can also develop secondary narcolepsy after an injury to the brain. (x)
Narcolepsy Symptoms
You usually begin to notice symptoms in your teenage years or early twenties. (x) However, many people can have symptoms for years before receiving a proper diagnosis. In most cases, the condition goes undiagnosed, and therefore patients do not receive appropriate treatment.
Narcolepsy is considered by some a lifelong problem that affects everyone differently. The most common symptoms are: (x)
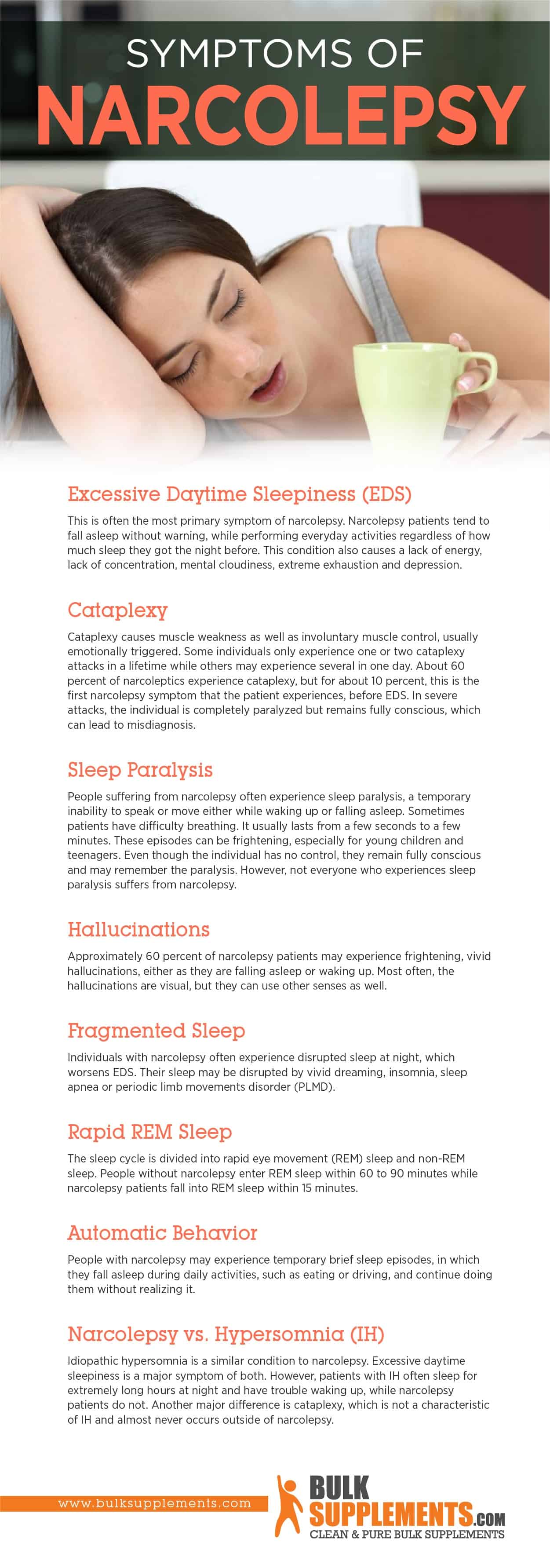
- Excessive Daytime Sleepiness (EDS)
EDS is often the most primary symptom of narcolepsy. Narcolepsy patients tend to fall asleep without warning while performing everyday activities, regardless of how much sleep they got the night before. This condition also causes a lack of energy, lack of concentration, mental cloudiness, extreme exhaustion and depression.
- Cataplexy
Cataplexy causes muscle weakness and involuntary muscle control, usually emotionally triggered. Some individuals only experience one or two cataplexy attacks in a lifetime, while others may experience several in one day. About 60 percent of narcoleptics experience cataplexy, but for about 10 percent, this is the first narcolepsy symptom that the patient experiences before EDS. (x) In severe attacks, the individual is wholly paralyzed but remains fully conscious, leading to misdiagnosis.
- Sleep Paralysis
People suffering from narcolepsy often experience sleep paralysis, a temporary inability to speak or move either while waking up or falling asleep. Sometimes patients have difficulty breathing. It usually lasts from a few seconds to a few minutes. These episodes can frighten you, especially for young children and teenagers. Even though the individual has no control, they remain fully conscious and may remember the paralysis. However, not everyone who experiences sleep paralysis suffers from narcolepsy. (x)
- Hallucinations
Approximately 60 percent of narcolepsy patients may experience frightening, vivid hallucinations, either as they fall asleep or waking up. Most often, the hallucinations are visual, but they can use other senses as well.
- Fragmented Sleep
Individuals with narcolepsy often experience disrupted sleep at night, which worsens EDS. Their sleep experience goes through disruptive vivid dreaming, insomnia, sleep apnea or periodic limb movements disorder (PLMD). (x) (x) (x)
- Rapid REM Sleep
The sleep cycle division begins with rapid eye movement (REM) sleep and non-REM sleep. People without narcolepsy enter REM sleep within 60 to 90 minutes, while narcolepsy patients fall into REM sleep within 15 minutes. (x) (x)
- Automatic Behavior
If you have narcolepsy, you may experience temporary brief sleep episodes, in which you fall asleep during daily activities, such as eating or driving and continue doing them without realizing it. (x)
Narcolepsy vs. Hypersomnia (IH)
Idiopathic hypersomnia is a similar condition to narcolepsy. Excessive daytime sleepiness is a prominent symptom of both. However, patients with IH often sleep for extremely long hours at night and have trouble waking up, while narcolepsy patients do not. Another significant difference is cataplexy, which is not a characteristic of IH and rarely occurs outside of narcolepsy. (x)
Risk Factors for Narcolepsy
Researchers do not know the exact cause of narcolepsy. They theorize that a hypocretin deficiency could cause it, and some believe it’s associated with specific genes that control nerve signals that trigger sleep and wake signals. The consensus is that genetics, coupled with environmental triggers, affect your body and cause hypocretin deficiency. Researchers have identified the following risk factors: (x)
- Brain Injuries
Although it is rare, narcolepsy can develop after traumatic brain injuries, tumors or other diseases that target areas that control sleep. (x)
- Autoimmune Disorders
If the patient experiences cataplexy, they have usually lost some of the nerve cells that produce hypocretin, resulting in a deficiency that research sometimes links to autoimmune disorders. For example, in narcolepsy, the immune system may mistakenly attack the cells that produce hypocretin. (x)
- Family History
Although narcolepsy is usually a sporadic disorder — meaning it rarely runs in families — research has supported the possibility that it is inheritable. People who have a family member who has had narcolepsy have up to 40 percent probability of developing the condition themselves. (x) Approximately 10 percent of people with narcolepsy and cataplexy have a relative with the same condition. (x)
Other Risk Factors
- Swine Flu (H1N1) Virus
Researchers have found a connection between narcolepsy and the swine flu (H1N1 FLU) virus. Some vaccinations block a receptor for hypocretin in people with a specific genetic makeup, and H1N1 infection has caused symptoms similar to narcolepsy. (x) (x)
- Heavy Alcohol Consumption
A case report suggested chronic alcohol consumption may induce narcolepsy. (x)
Diagnosing Narcolepsy
Narcolepsy symptoms may not be exclusive to that disorder, so it becomes confused with other sleep conditions. Cataplexy is the most specific symptom that doctors use to diagnose because it appears in almost no other disorder. Doctors use a physical exam or an exhaustive evaluation of the patient’s medical history and sleep history using the following tests: (x)
- Polysomnogram (PSG)
PSG records brain and muscle activity, eye movements and breathing overnight to determine if the patient falls into REM sleep early in the sleep cycle because of narcolepsy or another condition.
- Multiple Sleep Latency Test (MSLT)
MSLT measures how long it takes the patient to fall asleep and whether they enter the REM stage.
- Epworth Sleepiness Scale (ESS)
The ESS questionnaire determines how likely the patient is to fall asleep in different circumstances.
- Actigraphy
Actigraphy is a monitoring system worn on the wrist that documents sleep habits.
- Lumbar Puncture
The lumbar puncture test collects cerebrospinal fluid from the lumbar spine to measure hypocretin levels.
Treatment
Currently, there is no cure for narcolepsy, but behavioral treatments and medications aim to improve symptoms so that patients can improve daytime functioning and lead a more productive life. (x)
Medications for Narcolepsy
- Modafinil: Stimulates the central nervous system to reduce daytime drowsiness (x)
- Amphetamine-like stimulants: a second option to modafinil to reduce daytime sleepiness
- Sodium oxybate: treats cataplexy and EDS (x)
Lifestyle Remedies for Narcolepsy
Changing your lifestyle and health routine can help lessen the severity of narcolepsy and make it more manageable. Some lifestyle remedies include:
Supplements for Narcolepsy
There are not many recommended supplements for narcolepsy, but you might want to consider vitamins, herbs, proteins and supplements that help build up your body’s nervous and immune system.
Eating a balanced diet with plenty of fresh, clean water is also advised. Discuss this with your primary care physician. Supplements to consider taking:
- Vitamin B12
Eating foods rich in vitamin B12 — or supplementing — helps improve energy levels, mood and memory. According to the National Institute of Health, the suggested dosage for vitamin B12 powder is between 0.4 micrograms and 2.8 micrograms. (x)
- Vitamin D
A study found that people with narcolepsy had a high frequency of Vitamin D deficiency, which also causes pain and fatigue. (x) Vitamin D supplements are the best source of the nutrient.
Where to Buy Supplements for Narcolepsy?
You can purchase these supplements for Narcolepsy at BulkSupplements.com. The company is an industry-leading manufacturer and distributor of pure dietary supplements.
BulkSupplements.com is not just a consumer brand. It also supplies pure ingredients to other food and supplement brands to make their products. All products at BulkSupplements.com are manufactured and tested according to current and proper manufacturing practices.
Are you interested in trying any of these supplements mentioned in this article as a possible solution to helping you with Narcolepsy? Contact BulkSupplements.com to place an order today.
The Bottom Line
Narcolepsy is a chronic neurological disorder with no known cure or definite cause. It often occurs during childhood or early adolescence, but can strike at any time. It develops when your body cannot regulate sleep cycles, causing excessive sleepiness during the day.
The major symptom of narcolepsy is an inability to stay awake, even when undertaking daily activities like cooking and driving. Other symptoms include cataplexy, sleep paralysis and vivid and frightening hallucinations. Though there is no cure, patients can control their symptoms with medications and lifestyle changes to increase productivity.
Adding supplements to your diet as a way to manage the condition is not a bad idea. It may prove fruitful. Discuss vitamins and other supplements with your healthcare provider before you take any for your health concern.
These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure or prevent any disease.