What is Chloasma?
Chloasma is a temporary skin condition that appears as splotchy skin with large brown spots, mostly on the face. Chloasma, also known as the pregnancy mask, is thought to come about partially due to hormonal changes and affects 50 to 70 percent of pregnant women (x).
Also called melasma, the condition is not unique to pregnancy or women. Men and women can both develop chloasma, particularly if they have a family history of the condition and have a dark complexion.
Chloasma Characteristics
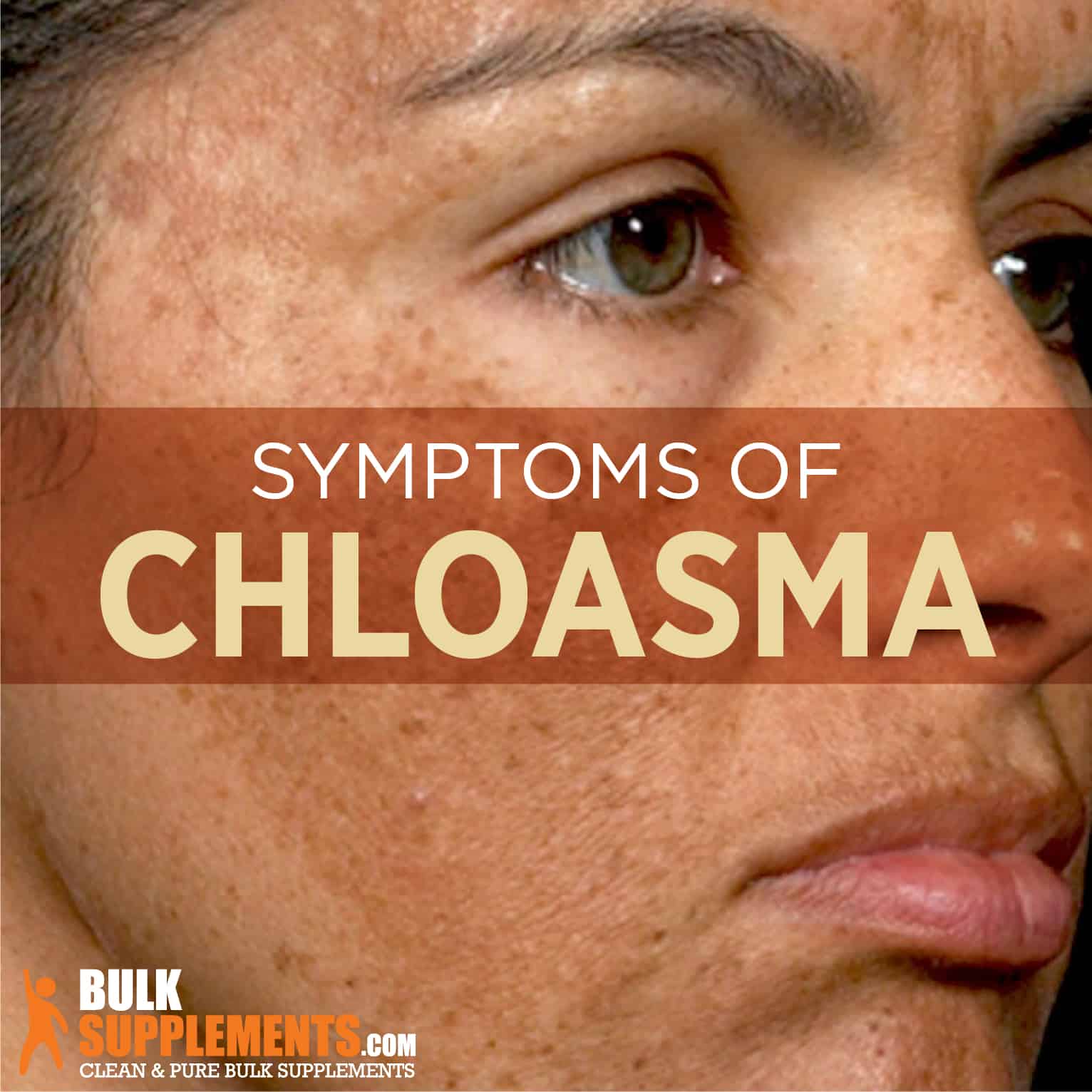
Chloasma has several characteristics, and not all people who experience the condition show the same ones. It typically appears as darkened spots on the skin that are roughly the same size and shape on both sides of the affected area.
These skin discolorations can show up anywhere on the body, but they appear often on the cheeks, upper lip, chin and forehead. Less frequently, they appear on the arms, chest and neck. Their symmetrical shape is like a mask, hence the term “pregnancy mask” (x).
Chloasma is a condition that can be seen, not felt. In fact, people with chloasma do not have any particular sensitivities in connection with the darkened skin. Also, there is no pain, discomfort or illness associated with chloasma. In fact, its only cause for concern is how it looks. Therefore, some people with chloasma do not like the way it looks on their skin and seek treatments to lighten the splotches.
Causes of Chloasma
The exact cause of chloasma is unknown and remains one of the mysteries of modern medicine and pregnancy. However, certain characteristics and conditions do correlate with the development of chloasma (x).
Melanin and Ultraviolet Rays
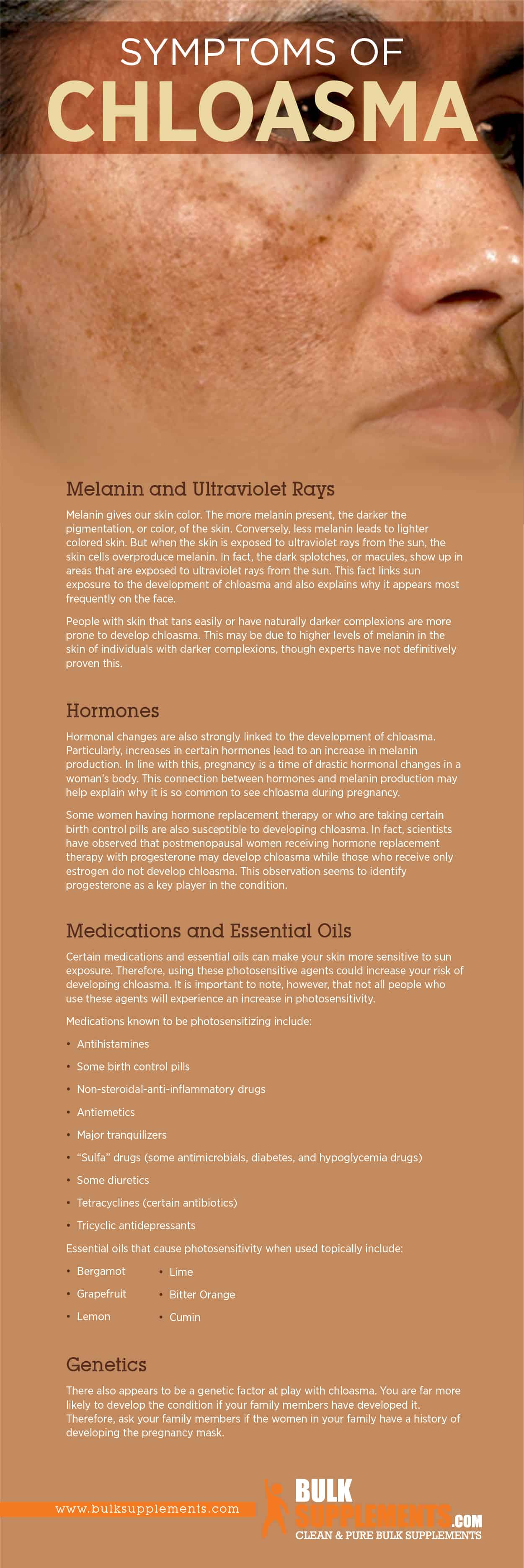
Melanin gives our skin color. The more melanin present, the darker the pigmentation, or color, of the skin. Conversely, less melanin leads to lighter colored skin. But when the skin is exposed to ultraviolet rays from the sun, the skin cells overproduce melanin. In fact, the dark splotches, or macules, show up in areas that are exposed to ultraviolet rays from the sun. This fact links sun exposure to the development of chloasma and also explains why it appears most frequently on the face.
People with skin that tans easily or have naturally darker complexions are more prone to develop chloasma. This may be due to higher levels of melanin in the skin of individuals with darker complexions, though experts have not definitively proven this (x).
Hormones
Hormonal changes are also strongly linked to the development of chloasma. Particularly, increases in certain hormones lead to an increase in melanin production. In line with this, pregnancy is a time of drastic hormonal changes in a woman’s body. This connection between hormones and melanin production may help explain why it is so common to see chloasma during pregnancy (x).
Some women having hormone replacement therapy or who are taking certain birth control pills are also susceptible to developing chloasma. In fact, scientists have observed that postmenopausal women receiving hormone replacement therapy with progesterone may develop chloasma while those who receive only estrogen do not develop chloasma. This observation seems to identify progesterone as a key player in the condition (x).
Medications and Essential Oils
Certain medications and essential oils can make your skin more sensitive to sun exposure. Therefore, using these photosensitive agents could increase your risk of developing chloasma. It is important to note, however, that not all people who use these agents will experience an increase in photosensitivity (x).
Medications known to be photosensitizing include (x):
- Antihistamines
- Some birth control pills
- Non-steroidal-anti-inflammatory drugs
- Antiemetics
- Major tranquilizers
- “Sulfa” drugs (some antimicrobials, diabetes, and hypoglycemia drugs)
- Some diuretics
- Tetracyclines (certain antibiotics)
- Tricyclic antidepressants
Essential oils that cause photosensitivity when used topically include (x):
- Bergamot
- Grapefruit
- Lemon
- Lime
- Bitter Orange
- Cumin
Genetics
There also appears to be a genetic factor at play with chloasma. You are far more likely to develop the condition if your family members have developed it. Therefore, ask your family members if the women in your family have a history of developing the pregnancy mask (x).
Did You Know?
- More cases of chloasma are diagnosed in the summertime compared to the rest of the year, possibly due to increased sun exposure (x).
- Melasma very rarely occurs before puberty, even if other conditions such as darker skin and sun exposure are present (x).
- Chloasma occurs more frequently in tropical climates than others.
- Although usually brown, the splotchy skin can also present as a blue-gray color (x).
Preventing Chloasma
The most important factor in the development of chloasma is sun exposure. Sun protection is the best means to avoid developing the condition in the first place. Although sunscreen will help some, it is best to take sun protection further if you have other risk factors for chloasma, such as family history or a dark complexion.
When you spend time in the sun, be sure to wear a wide-brimmed hat and sunglasses. You could also wear a long-sleeved rashguard style shirt that will protect your arms and chest from over-exposure.
Re-apply sunblock every two to four hours and seek the shade at regular intervals. Limit exposure to the sun as much as possible to prevent or lessen the symptoms of chloasma (x).
Chloasma Remedies and Supplements
The good news is that sometimes chloasma clears on its own if given sufficient time. The pregnancy mask can fade away after delivery, though it can take more than a year to do so. For those who do not wish to wait, there are supplements and treatments available worth considering. These natural remedies may speed the resolution of symptoms.
Zinc Glycinate Powder
Zinc is used for a variety of applications including digestive, immune and reproductive system support. It is also an ingredient commonly found in skin care products when combined with glycine, an amino acid that aids topical absorption. Zinc glycinate may boost collagen production, elastin production and lighten skin. These benefits can be beneficial in treating chloasma.
As a dietary supplement, try taking 90 mg daily with a meal, or as directed by your physician. Use a milligram scale for accurate measurement. Mix the powder into juice, water or a drink of your choosing.
Coconut Powder
Coconut powder is derived from young coconuts and is ultra-hydrating and antioxidant. It is an excellent addition to a post-workout recovery routine to regain hydration. It can also be used as a melasma treatment. Some with dark pigmentation have reported excellent results from using coconut oil.
As a drink supplement, mix one tablespoon into water, smoothies and other drinks. Alternatively, apply directly to the face by mixing a small amount of water with the powder to create a paste. Rub over dark areas in small circles to exfoliate and give time to allow penetration of the coconut to the skin.
Curcumin
Curcumin is derived from the spice turmeric and is touted for its varied health benefits. It brightens and lightens skin by suppressing a hormone that impacts melanin production (x). Antioxidant and anti-inflammatory properties also contribute to curcumin’s effectiveness as a skin supplement.
Curcumin can be taken orally by mixing with juice, water, or the drink of your choice. Curcumin is to be taken in one dose of 1,000 mg or less per day, depending on the intended effect. It should be taken along with water or a meal. Roughly, 1,000 mg for this product is equal to less than 1/2 tsp, or a little more than 3/8 tsp.
Apple Cider Vinegar
Apple cider vinegar has high amounts of glycol, which aid in clearing and lightening the skin. It helps slough off dead skin cells, remove impurities and leave your skin bright. You can wash your face with a mixture of apple cider vinegar and water, wipe it over your face like a toner or add it to a facial mask.
Topical Medical Treatments for Chloasma
The best creams for chloasma contain hydroquinone. This ingredient is effective because it impacts the formation, melanization and degradation of melanosomes. It is the “gold standard” for melasma treatment due to its depigmenting capabilities.
Azelaic acid is a component of topical creams to treat melasma and is desirable to those who experience adverse side effects to hydroquinone. A study showed that azelaic acid was just as effective as hydroquinone at reducing chloasma splotches (x). Further, it has been shown to lighten splotches faster and more completely than hydroquinone when combined with glycolic acid.
Retinoids were first used as an additional ingredient in creams containing hydroquinone to help improve penetration into the skin. Experts later discovered that retinoids work well at reducing chloasma on their own. The most effective treatments with retinoids contain other active ingredients such as steroids and hydroquinone.
Topical steroids are often turned to in dermatological applications as a means to reduce inflammation. They are sometimes included as part of a therapeutic cream for chloasma though how exactly they affect the pigmentation is not entirely understood (x).
Other Treatments for Chloasma
If supplements and topical treatments are not getting the results desired, a qualified dermatologist can perform targeted skin treatments that may help even the tone of the skin. Chemical peels, light treatments and laser resurfacing can all help restore a more even, consistent pigment to the skin.
The Bottom Line
Chloasma, or melasma, is a condition that predominantly affects women, many of whom are pregnant. This propensity to develop in pregnancy and the way the dark pigmentation appears symmetrically on the face led to the condition being called the pregnancy mask.
Although it is not medically necessary to treat chloasma because it doesn’t cause any pain or health problems, many people choose to treat chloasma for cosmetic reasons. Most people desire an even skin tone, especially on the face. When chloasma changes the look of the face, that is sufficient reason to seek treatment and resolution.
The condition is known to resolve without any intervention whatsoever spontaneously. But for those who wish to speed the process along, there are a multitude of natural and medical treatments available. Trial and error as well as utilizing several remedies in conjunction with one another may be necessary to find full resolution.